CAR T cell therapy is a new way to fight multiple myeloma. It uses your own immune system to attack cancer cells. This is a big hope for people with relapsed or refractory myeloma.
This therapy changes your T cells to find and kill myeloma cells. It’s a targeted treatment that has shown great results in trials. Some patients have even had long-term remissions.
This guide will explain CAR T cell therapy for multiple myeloma. We’ll cover how it works, who can get it, possible side effects, and new research. It’s important for patients, caregivers, and doctors to understand this treatment. It helps make informed choices and navigate the treatment journey.
Understanding CAR T Cell Therapy for Multiple Myeloma
CAR T cell therapy is a new targeted cellular therapy that uses a patient’s immune system to fight cancer. It has shown great promise in treating hematologic malignancies like multiple myeloma.
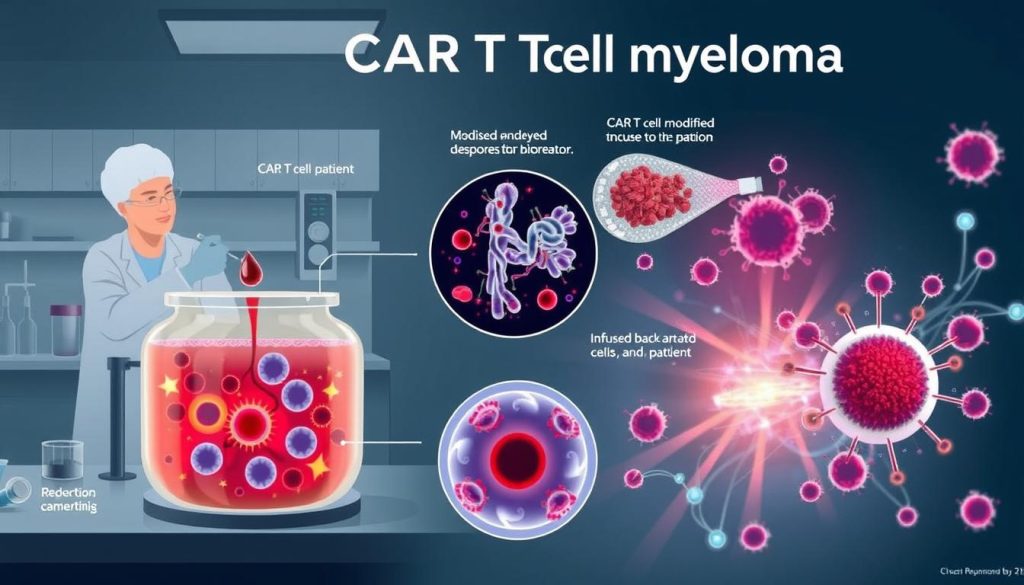
This therapy starts by collecting a patient’s T cells, a key type of white blood cell. These T cells are then modified in a lab. They are made to recognize and attack specific proteins on cancer cells.
The modified T cells are grown in the lab and given back to the patient. Inside the body, they find and kill cancer cells. This makes CAR T cell therapy a strong anti-cancer therapy.
“CAR T cell therapy represents a significant advancement in the treatment of multiple myeloma, providing hope to patients who have exhausted other treatment options.” – Dr. James L. Kochenderfer, National Cancer Institute
Many clinical trials have shown CAR T cell therapy’s success in treating multiple myeloma. Some patients have seen long-lasting benefits. Here are the results from a few trials:
| Clinical Trial | Overall Response Rate | Complete Response Rate |
|---|---|---|
| bb2121 (ide-cel) | 73% | 33% |
| JNJ-4528 (cilta-cel) | 97% | 67% |
| orvacabtagene autoleucel | 92% | 36% |
Even though CAR T cell therapy is very effective, it comes with challenges. It can cause side effects like cytokine release syndrome and neurological issues. These need careful monitoring and management. Also, researchers are studying how long the benefits last and when to use this therapy.
How CAR T Cell Therapy Works in Treating Multiple Myeloma
CAR T cell therapy is a new way to fight multiple myeloma. It uses the patient’s immune system to attack cancer cells. This method involves changing T cells to better target and destroy cancer.
First, T cells are taken from the patient’s blood. Then, these cells are changed in a lab to have special receptors. These receptors help the T cells find and attack myeloma cells.
Targeting Specific Antigens on Myeloma Cells
The main target for CAR T cell therapy in multiple myeloma is BCMA. BCMA is found on myeloma cells but not on healthy cells. This makes anti-BCMA CAR T cells very good at finding and killing myeloma cells without harming healthy tissues.
Researchers are also looking at other myeloma-specific antigens for CAR T cell therapy. These include:
- CD38
- SLAMF7
- CD19
- GPRC5D
“The ability to target specific antigens on myeloma cells is a major advantage of CAR T cell therapy. It allows for a highly targeted approach that can potentially lead to deep and durable responses in patients with multiple myeloma.” – Dr. James Kochenderfer, National Cancer Institute
Genetically Engineering T Cells for Enhanced Anti-Cancer Activity
After the T cells are changed and grown in the lab, they are given back to the patient. These genetically modified T cells can then find and attack myeloma cells.
These CAR T cells work better than regular T cells. They can keep fighting cancer for a long time. This could lead to long-term remission for patients with multiple myeloma.
Candidates for CAR T Cell Therapy in Multiple Myeloma
CAR T cell therapy is a new hope for those with relapsed refractory multiple myeloma. It uses the body’s immune system to fight cancer. This is a big deal for people with heavily pretreated myeloma.
Patient selection is key for CAR T cell therapy success. People who have tried many treatments before are usually considered. These treatments include proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies.
Relapsed or Refractory Multiple Myeloma Patients
Those with relapsed refractory multiple myeloma are the main candidates. They’ve seen their cancer come back after treatment or it hasn’t responded to therapy. CAR T cell therapy offers a new chance to manage their myeloma and improve their life.
“CAR T cell therapy has given me a second chance at life. After exhausting all other options, this treatment has been a beacon of hope in my battle against multiple myeloma.” – Maria, a CAR T cell therapy recipient
Eligibility Criteria for CAR T Cell Therapy
To qualify for CAR T cell therapy, patients must meet certain criteria. This includes:
- Confirmed diagnosis of relapsed refractory multiple myeloma
- Prior treatment with at least three lines of therapy, including a proteasome inhibitor, an immunomodulatory drug, and an anti-CD38 monoclonal antibody
- Adequate organ function, including heart, lung, liver, and kidney
- Absence of active infections or significant comorbidities that may interfere with treatment
Patient selection for CAR T cell therapy is a team effort. Hematologists, oncologists, and transplant specialists work together. They make sure the benefits outweigh the risks for each patient.
The Process of CAR T Cell Therapy for Multiple Myeloma
CAR T cell therapy for multiple myeloma is a detailed process. It starts with collecting the patient’s T cells through apheresis. This method draws blood, separates T cells, and then returns the blood to the patient.
After collecting T cells, they are genetically modified in a lab. This step uses viral vector transduction to add a gene for a chimeric antigen receptor (CAR). This allows the T cells to target specific antigens on myeloma cells. The modified T cells are then grown in the lab to prepare enough for treatment.
T Cell Collection and Genetic Modification
- Apheresis to collect the patient’s T cells
- Viral vector transduction to genetically modify T cells with CAR
- Multiplication of genetically modified T cells in the laboratory
Lymphodepletion and CAR T Cell Infusion
Before the CAR T cell infusion, patients get lymphodepleting chemotherapy. This reduces the number of immune cells in the body. It makes room for the CAR T cells to grow and lowers the chance of rejection. This chemotherapy lasts a few days.
After lymphodepletion, the patient gets the CAR T cell infusion. The modified T cells are given intravenously. They then spread throughout the body to find and attack myeloma cells.
Monitoring and Follow-Up Care
After the infusion, patients are watched for side effects and treatment results. Common side effects include:
- Cytokine release syndrome (CRS)
- Neurological toxicities
- Infection
- Low blood cell counts
Patients get support to handle side effects and are checked regularly. This care includes:
| Follow-up Care | Purpose |
|---|---|
| Blood tests | Monitor blood cell counts and myeloma markers |
| Imaging studies | Assess treatment response and detect any residual disease |
| Bone marrow biopsy | Evaluate the presence of myeloma cells in the bone marrow |
| Supportive care | Manage side effects and maintain quality of life |
The process of CAR T cell therapy for multiple myeloma is a testament to the advancements in medical science and the promise of personalized cancer treatment.
Knowing the steps of CAR T cell therapy helps patients and their families prepare. It allows them to work closely with their healthcare team for the best results.
Efficacy of CAR T Cell Therapy in Multiple Myeloma Clinical Trials
CAR T cell therapy is showing great promise in treating multiple myeloma. Clinical trials have seen high response rates and long periods without disease progression. This therapy also has the chance to wipe out remaining cancer cells.
In a recent trial, 85% of patients responded well to a CAR T cell therapy targeting BCMA. Half of them even achieved a complete response. The therapy also led to a median of 11.8 months without the disease getting worse.
Another trial tested a CAR T cell therapy that targets two proteins: BCMA and CD19. This approach resulted in a 95% response rate, with 50% of patients showing no cancer left. The median time without disease progression was 13.8 months, showing the therapy’s strong effect.
| Clinical Trial | Overall Response Rate | Complete Response Rate | Progression-Free Survival (median) |
|---|---|---|---|
| BCMA-targeted CAR T | 85% | 45% | 11.8 months |
| Dual-targeted (BCMA + CD19) CAR T | 95% | 50% | 13.8 months |
These results highlight CAR T cell therapy’s effectiveness in treating multiple myeloma. It offers new hope for those who have tried other treatments without success. The goal is to keep improving the therapy, aiming for even better outcomes for those fighting this disease.
Potential Side Effects and Risks of CAR T Cell Therapy
CAR T cell therapy is a new way to treat multiple myeloma. But, it’s important for patients to know about the possible side effects and risks. The main concerns are cytokine release syndrome (CRS) and neurological toxicities.
Cytokine Release Syndrome (CRS)
CRS is a common side effect of CAR T cell therapy, affecting up to 90% of patients. It happens when the immune system gets too active, releasing a lot of inflammatory cytokines. Symptoms can range from mild fever and fatigue to serious issues like hypotension, respiratory distress, and organ dysfunction.
Neurological Toxicities
Neurological toxicities, or ICANS, can also occur in patients. These can show up as confusion, delirium, aphasia, or seizures. The severity of ICANS can vary, with some patients having mild symptoms and others needing intensive care.

Strategies for Managing Side Effects
Healthcare providers use several strategies to manage CAR T cell therapy side effects. These include:
- Close monitoring of patients for signs and symptoms of CRS and ICANS
- Prompt administration of tocilizumab, an IL-6 receptor antagonist, to treat CRS
- Use of corticosteroids to manage severe CRS or ICANS unresponsive to tocilizumab
- Supportive care measures, such as fever management, fluid support, and respiratory assistance
The table below summarizes the key side effects and management strategies for CAR T cell therapy:
| Side Effect | Symptoms | Management Strategies |
|---|---|---|
| Cytokine Release Syndrome (CRS) | Fever, fatigue, hypotension, respiratory distress, organ dysfunction | Tocilizumab, corticosteroids, supportive care |
| Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) | Confusion, delirium, aphasia, seizures | Corticosteroids, supportive care |
By understanding the possible side effects and risks of CAR T cell therapy, patients and their caregivers can work closely with their healthcare team. This ensures prompt recognition and effective management of any complications that may arise during treatment.
FDA-Approved CAR T Cell Therapies for Multiple Myeloma
CAR T cell therapy has changed the game for multiple myeloma patients. It offers hope to those who’ve tried everything else. The U.S. Food and Drug Administration (FDA) has approved two CAR T cell therapies for multiple myeloma: idecabtagene vicleucel (Abecma) and ciltacabtagene autoleucel (Carvykti).
Idecabtagene vicleucel was developed by Bristol Myers Squibb and bluebird bio. It got FDA approval in March 2021. It’s for adults with relapsed or refractory multiple myeloma who’ve tried at least four treatments. This includes an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody.
The approval was based on the KarMMa clinical trial. It showed deep and durable responses in heavily pretreated patients.
Ciltacabtagene autoleucel was developed by Janssen Biotech. It got FDA approval in February 2022. It’s for adults with relapsed or refractory multiple myeloma who’ve tried at least four treatments. This includes a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody.
The approval was based on the CARTITUDE-1 clinical trial. It showed high response rates and prolonged progression-free survival in patients with heavily pretreated multiple myeloma.
“The FDA approval of idecabtagene vicleucel and ciltacabtagene autoleucel marks a significant milestone in the fight against multiple myeloma, providing patients with new hope and a powerful weapon against this devastating disease.”
Both therapies target the B-cell maturation antigen (BCMA). BCMA is a protein on the surface of multiple myeloma cells. By using genetically modified T cells to attack BCMA-expressing myeloma cells, these therapies have shown great results. They offer hope for long-term remission and improved quality of life for patients who’ve tried everything else.
Advantages of CAR T Cell Therapy Over Other Multiple Myeloma Treatments
CAR T cell therapy is a new way to fight cancer, unlike traditional treatments like chemotherapy. It uses the body’s immune system to attack cancer cells. This makes it a personalized cancer treatment for each person.
One big plus of CAR T cell therapy is how it targets and kills myeloma cells. It changes T cells to find and destroy myeloma cells. This helps keep healthy cells safe.
Targeted Approach to Eradicating Myeloma Cells
Unlike other treatments, CAR T cell therapy focuses on cancer cells. This makes it more effective at getting rid of myeloma cells. The T cells are made to find and kill cancer cells only.
“CAR T cell therapy represents a significant advance in the treatment of multiple myeloma, providing a targeted and potentially curative approach for patients who have exhausted other treatment options.” – Dr. James Kochenderfer, National Cancer Institute
Potential for Long-Term Remission
Another benefit of CAR T cell therapy is its chance to lead to long-term remission. Studies show some patients stay cancer-free for a long time. This is a big step forward in treating multiple myeloma.
| Treatment | Overall Response Rate | Complete Response Rate |
|---|---|---|
| CAR T Cell Therapy | 85-100% | 45-60% |
| Conventional Chemotherapy | 60-70% | 10-20% |
The table shows CAR T cell therapy beats traditional chemotherapy in treating multiple myeloma. It has better response rates. This means it could lead to better outcomes for patients.
Limitations and Challenges of CAR T Cell Therapy in Multiple Myeloma
CAR T cell therapy has shown promise in treating multiple myeloma. Yet, it faces several challenges. One major issue is antigen escape, where myeloma cells evade the CAR T cells. This can cause the treatment to fail over time.
The long time it takes to make CAR T cells is another big problem. It can take weeks to prepare the therapy. This delay can let the disease get worse. Researchers are working to make the process faster and to create ready-made CAR T cells.
The high cost of CAR T cell therapy is a major obstacle. It can cost over $400,000 per patient. This price is hard for many to afford. It shows the need for cheaper treatments.
| Limitation/Challenge | Description | Potential Solutions |
|---|---|---|
| Antigen escape | Myeloma cells lose or downregulate target antigen, reducing CAR T cell effectiveness | Develop multi-antigen targeting CAR T cells or combination therapies |
| Manufacturing time | Lengthy process of collecting, modifying, and expanding patient’s T cells | Streamline manufacturing process and develop “off-the-shelf” CAR T cell products |
| Cost of treatment | High cost due to complex manufacturing process and personalized nature of therapy | Develop more affordable treatment options and improve insurance coverage |
Despite the hurdles, researchers and doctors are pushing forward. They aim to improve CAR T cell therapy for multiple myeloma. They’re working on new CAR T cells, faster production, and cheaper options. The goal is to make the treatment more accessible to those who need it.
Current Research and Future Directions in CAR T Cell Therapy for Multiple Myeloma
Researchers are working hard to make CAR T cell therapy better for treating multiple myeloma. They want to make CAR T cells more effective and last longer. They’re also looking into new ways to target cancer cells and combining therapies for better results.
Improving CAR T Cell Persistence and Efficacy
Scientists are creating next-generation CAR T cells to solve the problems of short-lived and less effective cells. They’re adding extra parts and making genetic changes to make these cells stronger and longer-lasting. This could help CAR T cells fight cancer better and for longer.

Developing New CAR T Cell Targets
Most CAR T cell treatments for multiple myeloma target BCMA. But researchers are looking at other targets to make treatment more effective. They’re working on CAR T cells that can target two antigens at once to fight cancer better. Some new targets being explored include:
- CD19
- CD38
- GPRC5D
- SLAMF7
Combining CAR T Cell Therapy with Other Treatments
Researchers are also looking into combining CAR T cell therapy with other treatments. This could make treatment more effective and last longer. Some promising combinations include:
| Combination Therapy | Rationale |
|---|---|
| CAR T cells + immunomodulatory drugs (IMiDs) | Augment immune response and enhance CAR T cell function |
| CAR T cells + checkpoint inhibitors | Counteract immunosuppressive tumor microenvironment |
| CAR T cells + targeted therapies (e.g., proteasome inhibitors) | Synergistic anti-myeloma activity and improved depth of response |
These new ideas could change how we treat multiple myeloma. They offer hope for better treatment outcomes and a better quality of life for patients. With ongoing research, the future of CAR T cell therapy looks bright for those fighting this tough cancer.
Patient Stories: Real-Life Experiences with CAR T Cell Therapy for Multiple Myeloma
CAR T cell therapy is showing great promise in treating multiple myeloma. Patient testimonials give us a look at how this treatment is changing lives. These stories highlight the treatment journey and the hope for a better quality of life for those fighting this tough blood cancer.
“CAR T cell therapy gave me a second chance at life. After years of struggling with multiple myeloma, I found hope in this targeted treatment.” – Sarah, multiple myeloma survivor
Many patients choose CAR T cell therapy after trying other treatments. The process is tough but offers a chance for remission and a return to normal life.
During the treatment journey, patients find strength in family support and their healthcare team’s dedication. The close care during CAR T cell therapy helps manage side effects, focusing on recovery.
“The support from my family and medical team was incredible. They were with me every step, celebrating milestones and helping through tough times.” – Michael, CAR T cell therapy recipient
More patient stories show CAR T cell therapy’s power to improve quality of life for multiple myeloma patients. These patient testimonials offer hope to others on their cancer journey. They show that CAR T cell therapy is making a big difference in multiple myeloma care.
Accessing CAR T Cell Therapy for Multiple Myeloma
Getting CAR T cell therapy for multiple myeloma starts with a referral from your oncologist. This referral goes to a certified treatment center. These places have the skills and tools needed to give this treatment safely and well.
The referral process checks your medical history and health status. It also sees if you’re a good fit for CAR T cell therapy. If you’re in, you’ll team up with healthcare pros at the center to get ready for the treatment.
Insurance coverage for CAR T cell therapy can change based on your plan and the center’s rules. Many insurances, like Medicare and Medicaid, help pay for this treatment. But, it’s key to talk with your healthcare team and insurance about what you’ll pay.
Patient Assistance Programs
If money is a worry for CAR T cell therapy, there are patient assistance programs to help. These come from drug companies, non-profits, and government groups. They can help with costs like:
- Medication costs
- Travel and lodging
- Co-pays and deductibles
“Accessing CAR T cell therapy can be a complex process, but with the right support and resources, patients can navigate the journey with greater ease and confidence.” – Dr. Sarah Thompson, oncologist and CAR T cell therapy specialist
By teaming up with your healthcare team and looking into financial help, patients with multiple myeloma can get CAR T cell therapy. This can greatly improve their health and life quality.
Preparing for CAR T Cell Therapy: What Patients Should Know
Starting CAR T cell therapy for multiple myeloma is a big step. Patient education and preparation are key for a good experience. Knowing what to expect and how to prepare can reduce stress and make the process easier.
Before starting CAR T cell therapy, you’ll have a detailed pre-treatment evaluation. This checks your health and if you’re a good candidate for the treatment. The evaluation might include:
- Physical examination
- Blood tests
- Bone marrow biopsy
- Imaging studies (e.g., PET/CT scans)
- Cardiac and pulmonary function tests
Your healthcare team will give you lots of patient education materials. These will explain the therapy, possible side effects, and what to do after treatment. It’s important to ask questions and share any worries you have.
Caregiver support is very important during CAR T cell therapy. Choose someone to help you with appointments, medicine, and emotional support. They should also understand the treatment and any possible problems.
“Having a strong support system was critical during my CAR T cell therapy. My family and friends were there every step of the way, giving encouragement and practical help.”
Here are some practical things to do before CAR T cell therapy:
- Make plans for getting to and from the treatment center
- Book a place to stay near the treatment center, if needed
- Plan for work and family duties during treatment
- Check your insurance and look into financial help options
By educating yourself, going through evaluations, and building a strong support system, you can face CAR T cell therapy with confidence. Your healthcare team will help you through every part of this promising treatment for multiple myeloma.
Caregiving and Support During CAR T Cell Therapy for Multiple Myeloma
When a loved one gets CAR T cell therapy for multiple myeloma, the caregiver role is key. They offer emotional support and practical assistance. Caregivers help patients face the challenges of this new treatment, giving comfort and support every step of the way.
Emotional support is a big part of caregiving during CAR T cell therapy. Patients might feel scared, anxious, or unsure. Caregivers can help by:
- Listening well and creating a safe space for feelings
- Sharing words of encouragement and reassurance
- Doing relaxing things together, like reading or watching movies
- Helping find support groups or counseling, if needed
Caregivers also give practical help. This includes:
- Going to medical appointments and treatment sessions with patients
- Helping with medicine and watching for side effects
- Doing daily tasks, like cooking, cleaning, and running errands
- Talking to the healthcare team and keeping family updated
It’s important for caregivers to take care of themselves too. Caring for someone getting CAR T cell therapy can be tough. Caregivers should:
Remember to take care of yourself, too. You can’t pour from an empty cup. Take breaks, seek support, and do things that make you happy and relaxed.
Caring for someone during CAR T cell therapy for multiple myeloma shows deep love and commitment. By giving emotional support and practical help, caregivers are a big part of the treatment journey. They help patients stay hopeful, strong, and positive as they face this new treatment.
Long-Term Outlook and Survivorship After CAR T Cell Therapy
As CAR T cell therapy shows promise in treating multiple myeloma, it’s key for patients and doctors to think about the long-term. This treatment could lead to long-term remission. Patients need to be ready for the challenges and chances that come with life after treatment.
One important part of long-term survivorship is watching for relapse and late effects. CAR T cell therapy has shown great results in getting rid of cancer. But, patients must stay alert and have regular check-ups to catch any signs of cancer coming back. It’s also vital to watch for late effects, like long-lasting low blood counts or new cancers, which can happen months or years later.
Monitoring for Relapse and Late Effects
To keep an eye on relapse and late effects, patients should:
- Go to regular check-ups with their oncologist and healthcare team
- Have blood tests, bone marrow biopsies, and imaging studies as needed
- Tell their healthcare provider right away if they notice any new or lasting symptoms
Maintaining Quality of Life After Treatment
It’s also important to focus on keeping quality of life after CAR T cell therapy. Patients may face physical, emotional, and social challenges as they adjust to life after treatment. To help their well-being, patients should:
- Stay active and eat healthy
- Get support from family, friends, and support groups
- Deal with any lasting side effects or problems with their healthcare team
- Make a survivorship care plan with their oncologist
A detailed survivorship care plan is a key tool for life after CAR T cell therapy. This plan should include a summary of treatment, a schedule for follow-ups, and tips for staying healthy. By working with their healthcare team and following their care plan, patients can improve their long-term health and quality of life after this innovative treatment.
“CAR T cell therapy has given me a second chance at life, and I am determined to make the most of it. By staying proactive about my health and embracing the support of my loved ones, I am confident that I can thrive in my post-treatment journey.” – Sarah, CAR T cell therapy survivor
CAR T Cell Therapy Multiple Myeloma: A Promising Advance in Myeloma Treatment
CAR T cell therapy is a new way to fight cancer, changing how we treat multiple myeloma. It uses a patient’s immune system to attack cancer cells. This method has shown great success in clinical trials, bringing hope to those with relapsed or refractory myeloma.
As research improves, the future of treating myeloma looks brighter. CAR T cell therapy could lead to long-term remission and targeted cancer cell destruction. This could greatly improve survival rates and quality of life for those with the disease.
Despite challenges like managing side effects, the field is advancing fast. Researchers and healthcare teams are working hard to improve myeloma care. It’s important to support research, increase access to CAR T cell therapy, and help patients and their families. With CAR T cell therapy, we’re entering a new era in treating multiple myeloma, full of hope and better outcomes.
FAQ
Q: What is CAR T cell therapy for multiple myeloma?
A: CAR T cell therapy is a new way to fight cancer. It uses your own immune cells to attack cancer cells. This method changes T cells to find and destroy myeloma cells more effectively.
Q: Who is eligible for CAR T cell therapy in multiple myeloma?
A: This therapy is for those with cancer that has come back or not responded to other treatments. Who can get it depends on the treatment and the patient’s health.
Q: How does the CAR T cell therapy process work?
A: First, T cells are taken from the patient. Then, they are changed to find and kill myeloma cells. After chemotherapy, these changed cells are put back into the patient. The patient is watched for side effects and how well the treatment works.
Q: What are the possible side effects of CAR T cell therapy?
A: Side effects can be mild or severe. They include problems with cytokines and the nervous system. Doctors use special drugs and care to help manage these issues.
Q: Are there any FDA-approved CAR T cell therapies for multiple myeloma?
A: Yes, two therapies are approved by the FDA. Idecabtagene vicleucel (Abecma) and ciltacabtagene autoleucel (Carvykti) are for patients who have tried many treatments.
Q: How effective is CAR T cell therapy in treating multiple myeloma?
A: Studies show it works well. Patients often see their cancer shrink a lot. It can also help them live longer without the cancer coming back.
Q: What are the advantages of CAR T cell therapy compared to other myeloma treatments?
A: It targets cancer cells directly. This can lead to better and longer-lasting results. It might even help some patients stay cancer-free for a long time.
Q: What are the limitations and challenges of CAR T cell therapy in multiple myeloma?
A: It might not work for everyone. Making the T cells takes time. It’s also very expensive. Researchers are working to make it better and more affordable.
Q: How can patients access CAR T cell therapy for multiple myeloma?
A: Talk to your doctor to see if you’re a good candidate. You’ll need to go to a certified center. Insurance and financial help are important too.
Q: What is the long-term outlook for patients receiving CAR T cell therapy for multiple myeloma?
A: The outlook is good. Patients can have long-lasting remissions and better quality of life. But, they need to stay on top of their health and follow care plans.