Chimeric antigen receptor (CAR) T-cell therapy is a new way to fight cancer. It uses your own immune system to attack cancer cells. This method changes T-cells, a type of white blood cell, to target cancer cells.
Understanding CAR T-cell therapy is key for patients. This guide will cover everything from the first visit to aftercare. You’ll learn about the steps from getting your T-cells to the infusion and follow-up care.
We want to give you a clear view of your CAR T-cell therapy journey. This way, you can make informed decisions and work well with your healthcare team. Let’s dive into the world of CAR T-cell therapy and its promise for cancer patients.
Introduction to CAR T-Cell Therapy
Cancer immunotherapy has changed how we treat cancer. CAR T-cell therapy is a key part of this change. It uses a patient’s immune system to fight cancer, giving hope to those with blood cancers.
This therapy works by changing T-cells to find and kill cancer cells. T-cells are a type of white blood cell. They are made to recognize and attack cancer cells.
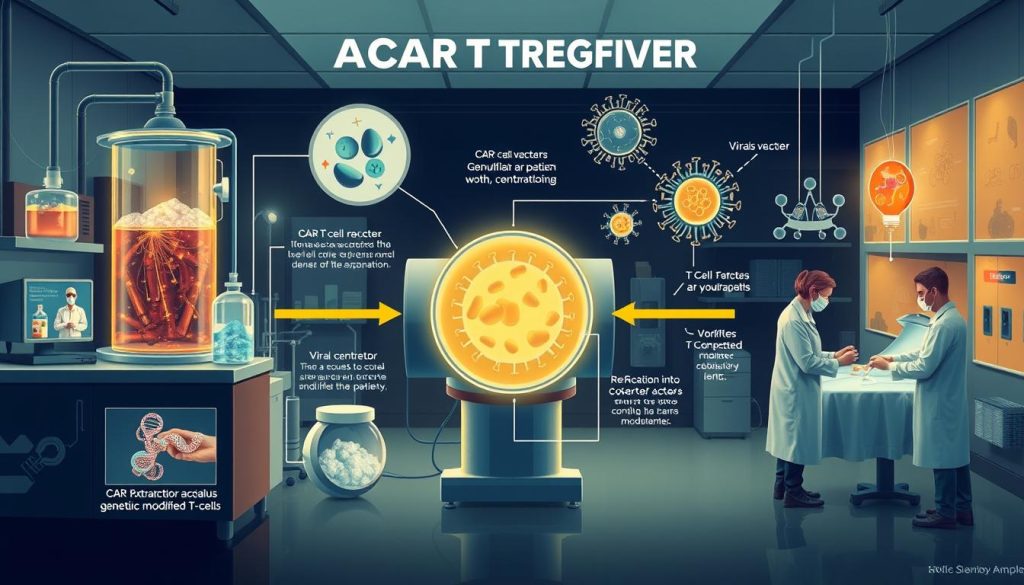
The therapy starts with taking T-cells from a patient. These cells are then changed in a lab to find cancer cells. After, they are given back to the patient to fight cancer.
What makes CAR T-cell therapy special is its precision. It targets cancer cells well, without harming healthy cells. This has shown great results in treating blood cancers like:
- Acute Lymphoblastic Leukemia (ALL)
- Diffuse Large B-Cell Lymphoma (DLBCL)
- Multiple Myeloma
Even though CAR T-cell therapy is promising, it comes with risks. Side effects like cytokine release syndrome and neurotoxicity can happen. These need careful watching and management by medical experts.
Scientists are working hard to make CAR T-cell therapy work for more cancers. This could change cancer treatment a lot. It could give new hope to patients who have tried other treatments.
How CAR T-Cell Therapy Works
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. This method changes the patient’s T-cells to better target and kill cancer.
Targeting Cancer Cells with Engineered T-Cells
The journey starts with taking a sample of T-cells from the patient. This is done through a process called leukapheresis. The T-cells are then sent to a lab for genetic changes.
In the lab, scientists add a gene for a chimeric antigen receptor (CAR) to the T-cells. This receptor helps the T-cells find and attach to cancer cells.
After the T-cells are modified, they are grown into millions of cancer-fighting cells. These CAR T-cells are then given back to the patient. They can then find and destroy cancer cells in the body.
The Role of Chimeric Antigen Receptors (CARs)
Chimeric antigen receptors are key to CAR T-cell therapy’s success. They are made to recognize proteins on cancer cells but not on healthy cells. This helps CAR T-cells target cancer cells without harming healthy tissue.
“The development of CAR T-cell therapy has opened up new possibilities in the fight against cancer, giving hope to patients who have tried other treatments.”
A CAR has three main parts:
| Component | Function |
|---|---|
| Antigen-binding domain | Recognizes and binds to the target antigen on the cancer cell surface |
| Transmembrane domain | Anchors the CAR to the T-cell membrane |
| Signaling domain | Activates the T-cell upon antigen binding, triggering its cancer-fighting functions |
Choosing the right antigen is very important for CAR T-cell therapy. Researchers pick antigens that are common on cancer cells but rare on healthy cells. This ensures the treatment is effective and safe.
Pre-Treatment Evaluation and Preparation
Before starting CAR T-cell therapy, patients go through a detailed check-up. This check-up is to see if they can have the treatment. It makes sure they are healthy enough and that their cancer might respond well.
The first thing is a full medical check. This includes a physical exam, blood tests, and scans like CT or PET. These help doctors understand the patient’s health and how big their cancer is.
Patients also have tests to check their immune system. These tests are:
- Lymphocyte count: This checks the number of T-cells in the blood. T-cells are key for CAR T-cell therapy.
- Cytokine levels: Cytokines are proteins that help the immune system. Testing them shows how well the patient’s immune system will work with CAR T-cells.
- Viral testing: Patients are checked for viruses like HIV and hepatitis B and C. These could affect their treatment eligibility.
“The pre-treatment evaluation is a critical step in the CAR T-cell therapy process. It allows us to carefully select patients who are most likely to benefit from the treatment while minimizing possible risks.”
– Dr. Sarah Johnson, oncologist
After being found eligible, patients start getting ready for the treatment. They might change their medicines, get vaccines, or have more tests. This is to make sure they are as healthy as possible before starting therapy.
Leukapheresis: Collecting the Patient’s T-Cells
The first step in CAR T-cell therapy is collecting T-cells through leukapheresis. Blood is drawn from the patient, and T-cells are separated from other blood parts. The blood without T-cells is then returned to the patient.
The Leukapheresis Procedure
Leukapheresis happens in a hospital or outpatient setting. It takes several hours. The patient is connected to a machine via an IV line.
Blood is drawn from one arm, processed, and then returned to the other arm. During this, patients can relax or read. They might feel a bit tired or lightheaded, but these feelings go away soon.

After the procedure, the T-cells are ready for the next step in CAR T-cell therapy.
Processing and Shipping the Collected T-Cells
After collecting, the T-cells are processed and prepared for shipping. They are washed, concentrated, and cryopreserved for safe transport.
The T-cells are then packaged and shipped to a manufacturing facility. They are kept at the right temperature during transport. This ensures they stay viable for the next step: genetically engineering the T-cells to fight cancer.
| Leukapheresis Process Step | Description |
|---|---|
| Blood Draw | Blood is drawn from the patient’s arm and circulated through the leukapheresis machine |
| T-Cell Collection | The leukapheresis machine separates and collects T-cells from the blood |
| Blood Return | The remaining blood components are returned to the patient’s body through the other arm |
| T-Cell Processing | The collected T-cells are washed, concentrated, and cryopreserved for shipping |
Manufacturing the CAR T-Cells
The process of making CAR T-cells is complex and requires special skills. It involves changing the patient’s T-cells to fight cancer. This step is key in the CAR T-cell therapy process and needs advanced technology and knowledge.
Genetically Engineering the T-Cells
First, the patient’s T-cells are collected through a process called leukapheresis. Then, they are sent to a special place where the car t-cell production starts. The T-cells are changed to have a special receptor on their surface.
This receptor helps the T-cells find and attack cancer cells. A virus carries the gene for this receptor into the T-cells. This is called car t-cell transfection.
- An antigen-binding domain that recognizes and binds to a specific protein on the surface of cancer cells
- A hinge region that provides flexibility and helps the CAR to orient properly
- A transmembrane domain that anchors the CAR to the T-cell membrane
- Intracellular signaling domains that activate the T-cell when the CAR binds to its target
Expansion and Multiplication of CAR T-Cells
After the T-cells are changed, they start to grow and multiply. This is done by adding growth factors and other helpers. The goal is to have enough CAR T-cells for the treatment.
The process can take weeks, as shown in the table below:
| Manufacturing Step | Duration |
|---|---|
| Genetic modification of T-cells | 3-5 days |
| Expansion of CAR T-cells | 10-14 days |
| Quality control testing | 3-5 days |
| Total manufacturing time | 2-4 weeks |
The CAR T-cell manufacturing process is a testament to the incredible advances in biotechnology and cell therapy that have made this innovative treatment possible.
Once the CAR T-cells are ready and checked, they are frozen and sent back to the treatment center. There, they are thawed and given to the patient.
Lymphodepletion: Preparing the Patient’s Body
Before CAR T-cell therapy, patients go through a key step called lymphodepletion. This involves a short chemotherapy before CAR T-cell therapy. It makes the body ready for the modified T-cells to fight cancer cells well.

The main goal of lymphodepletion is to lower the number of immune cells, like T-cells. This creates space for the CAR T-cells to grow and work without being blocked by the body’s own T-cells.
Lymphodepletion happens a few days before the CAR T-cell infusion. The chemotherapy used can change based on the CAR T-cell product and the patient’s health. Common drugs include:
- Fludarabine
- Cyclophosphamide
- Bendamustine
Lymphodepletion is key for CAR T-cell therapy to work. But, it can cause side effects like regular chemotherapy. Patients might feel:
- Fatigue
- Nausea and vomiting
- Decreased blood cell counts
- Increased risk of infections
“Lymphodepletion is a critical step in preparing my body for CAR T-cell therapy. Though the chemotherapy side effects are tough, I know it’s needed for the engineered T-cells to fight my cancer.”
– Sarah, CAR T-cell therapy patient
To keep patients safe, they are watched closely during and after lymphodepletion. They get help to manage side effects and prevent infections. After lymphodepletion, they are ready for the CAR T-cell infusion.
CAR T-Cell Infusion: Administering the Treatment
After the patient has gone through lymphodepletion and the CAR T-cells are made, the next step is to put the cells back into the patient’s body. This important step is when the CAR T-cells are given to the patient. The patient is watched closely during and after this.
The Infusion Process
The car t-cell infusion happens in a hospital, either in an outpatient clinic or an inpatient unit. The CAR T-cells are given through an IV, like a blood transfusion or chemotherapy. The time it takes can vary, but it’s usually between 30 minutes to an hour.
While getting the infusion, patients are watched by healthcare professionals. They check things like blood pressure and heart rate. Patients might feel a little sick, like fever or nausea, but these can be treated.
Monitoring During and After Infusion
After the car t-cell infusion, patients are watched for days to weeks. This is to catch and handle any side effects or problems. Patients usually have to stay near the treatment center for at least 4 weeks.
During this time, patients get regular checks. These include:
- Physical exams
- Blood tests to check cell counts and organ function
- Imaging studies to see how the treatment is working and if there’s any toxicity
The healthcare team keeps an eye out for cytokine release syndrome (CRS) and neurotoxicity. These are serious side effects of CAR T-cell therapy. Here’s a table showing the CRS grading system:
| Grade | Symptoms | Management |
|---|---|---|
| 1 | Mild fever, fatigue, headache | Supportive care, antipyretics |
| 2 | Moderate fever, hypotension, hypoxia | Intravenous fluids, oxygen support, tocilizumab |
| 3 | High fever, severe hypotension, respiratory distress | Intensive care unit admission, vasopressors, high-dose steroids |
| 4 | Life-threatening complications, multi-organ failure | Aggressive intensive care support, immunosuppression |
By watching patients closely during and after the car t-cell infusion, healthcare providers can quickly spot and handle any bad reactions. This makes sure patients stay safe and comfortable during the treatment administration process.
Potential Side Effects and Their Management
CAR T-cell therapy is a promising treatment for some blood cancers. But, it’s important for patients and their families to know about possible side effects. The main concerns are cytokine release syndrome (CRS) and neurotoxicity. It’s key for doctors to quickly spot and manage these issues to keep patients safe and help them get better.

Cytokine Release Syndrome (CRS)
CRS happens when the immune system, including CAR T-cells, releases a lot of inflammatory molecules. Symptoms can be mild, like flu-like symptoms, or severe, like organ problems. Doctors watch for signs of CRS and use medicines like tocilizumab and corticosteroids to lower inflammation.
Neurotoxicity
Neurotoxicity, or ICANS, is another side effect of CAR T-cell therapy. Symptoms include confusion, trouble speaking, and seizures. Doctors check for these signs and use supportive care and corticosteroids to help the brain.
Other Possible Side Effects
Patients may also face other side effects, like infections and blood problems. These can include fever, chills, and anemia. Doctors closely watch for these and provide the right care and treatment.
| Side Effect | Symptoms | Management |
|---|---|---|
| Infection | Fever, chills, cough, fatigue | Antibiotics, antifungals, antivirals |
| Anemia | Fatigue, pale skin, shortness of breath | Blood transfusions, erythropoiesis-stimulating agents |
| Thrombocytopenia | Easy bruising, petechiae, bleeding | Platelet transfusions |
Doctors keep a close eye on patients for these and other side effects. They provide the needed care and treatment. Even with the risks, many find the benefits of CAR T-cell therapy worth it.
Post-Treatment Monitoring and Follow-Up
After CAR T-cell therapy, patients start a critical phase of care. This phase is key for checking how well the treatment works and managing side effects. Regular visits with the medical team are vital.
The number of follow-up visits can change based on the patient’s needs and how they react to the therapy. At first, patients see their doctors more often. As time goes on, the visits become less frequent. During these visits, doctors will do many tests and checks.
- Physical examinations
- Blood tests to monitor cell counts and immune function
- Imaging scans (e.g., CT, PET, or MRI) to evaluate treatment response
- Assessment of any lingering side effects or complications
Patients also get a personalized care plan. This plan includes tips for a healthy lifestyle and how to avoid infections. It also tells patients when to contact their doctors if they have concerns.
“Long-term monitoring is a vital aspect of CAR T-cell therapy, as it allows us to ensure the best possible outcomes for our patients. We work closely with each individual to develop a comprehensive follow-up plan that meets their unique needs.”
Good communication between patients and their doctors is key during follow-up. Patients should talk openly about any worries or questions. This helps doctors quickly address any issues and adjust the care plan as needed.
| Follow-up Timeline | Frequency of Appointments | Key Assessments |
|---|---|---|
| First 3 months | Every 1-2 weeks | Physical exam, blood tests, imaging scans |
| 3-6 months | Every 4-6 weeks | Physical exam, blood tests, imaging scans |
| 6-12 months | Every 2-3 months | Physical exam, blood tests, imaging scans |
| Beyond 1 year | Every 3-6 months | Physical exam, blood tests, imaging scans as needed |
By following the post-treatment plan, patients can improve their recovery and long-term health after CAR T-cell therapy. This detailed approach to car t-cell therapy follow-up and long-term monitoring ensures patients get the support they need for the best outcomes.
Car T-Cell Therapy Process: Step-by-Step Overview
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. The car t-cell therapy timeline has key steps, from the first check-up to the last follow-up. Here’s a quick look at the treatment process:
- Pre-treatment evaluation: Doctors check if the patient can get CAR T-cell therapy and do tests.
- Leukapheresis: T-cells are taken from the patient’s blood. This process separates white blood cells.
- Manufacturing: The T-cells are changed to find and kill cancer cells. Then, they are grown in a lab.
- Lymphodepletion: The patient gets chemotherapy to lower immune cells. This makes room for the CAR T-cells.
- CAR T-cell infusion: The CAR T-cells are put back into the patient’s blood. They then find and kill cancer cells.
- Monitoring and management: The patient is watched for side effects like CRS and neurotoxicity. The medical team handles these.
- Follow-up: The patient is checked regularly for how well the treatment is working and any lasting side effects.
“CAR T-cell therapy offers hope to patients with certain types of blood cancers who have exhausted other treatment options. The step-by-step process, while complex, is carefully designed to maximize the treatment’s effectiveness and minimize risks.”
During the car t-cell therapy timeline, patients get help from many healthcare professionals. This includes doctors, nurses, and social workers. Knowing the treatment process overview helps patients prepare and make informed choices about their care.
Success Stories and Patient Experiences
CAR T-cell therapy has changed many cancer patients’ lives. It offers hope and a chance at remission when other treatments fail. Here, we share inspiring car t-cell therapy success stories and patient testimonials. They show the amazing promise of this new treatment.
“I was diagnosed with advanced lymphoma and had exhausted all conventional treatment options. CAR T-cell therapy was my last hope, and it saved my life. Today, I am cancer-free and grateful for every moment.”
– Sarah, CAR T-cell therapy recipient
Many patients have seen remarkable results from CAR T-cell therapy. Some even achieve complete remission after just one infusion. These stories are a beacon of hope for those facing cancer.
Patient testimonials also reveal the emotional and physical journey of CAR T-cell therapy. The process can be tough, with side effects like cytokine release syndrome and neurotoxicity. Yet, patients say the benefits are worth the temporary discomfort.
“The CAR T-cell therapy process was intense, but the medical team was incredibly supportive every step of the way. The moment I learned that my cancer was in remission, all the challenges I faced during treatment became a distant memory. I am forever grateful for this life-saving therapy.”
– Michael, CAR T-cell therapy survivor
As more patients share their car t-cell therapy success stories, awareness grows. These personal accounts comfort and encourage those considering CAR T-cell therapy. They also underscore the need for ongoing research and development in this field.
Ongoing Research and Future Developments in CAR T-Cell Therapy
Researchers are working hard to make CAR T-cell therapy better. They want to help more people with cancer. This therapy has shown great results in treating some blood cancers.

Expanding CAR T-Cell Therapy to Other Cancer Types
Right now, CAR T-cell therapy mainly helps with blood cancers. But scientists are looking into using it for solid tumors too. They’re making new CAR designs to target specific antigens on solid tumor cells.
| Cancer Type | Target Antigen |
|---|---|
| Breast Cancer | HER2 |
| Prostate Cancer | PSMA |
| Glioblastoma | EGFRvIII |
Improving Safety and Efficacy
Researchers are also working to make CAR T-cell therapy safer and more effective. They want to reduce severe side effects like cytokine release syndrome (CRS) and neurotoxicity. Some ideas include:
- Incorporating safety switches that can deactivate CAR T-cells if necessary
- Developing CAR T-cells with lower affinity for target antigens to reduce overstimulation
- Using combination therapies to enhance the anti-tumor response while minimizing toxicity
Off-the-Shelf CAR T-Cell Therapies
Now, CAR T-cell therapy is made for each patient. But, researchers are making off-the-shelf car t-cells from healthy donors. These “universal” CAR T-cells could be available for anyone, making treatment faster and cheaper.
“The development of off-the-shelf CAR T-cell therapies has the power to change cancer treatment. It could make it more accessible and affordable for people all over the world.” – Dr. Michel Sadelain, Memorial Sloan Kettering Cancer Center
As car t-cell therapy research keeps moving forward, we’re looking at a future where this treatment helps more people. It will be safer, more effective, and easier to get, thanks to off-the-shelf car t-cells.
Accessing CAR T-Cell Therapy: Eligibility and Availability
CAR T-cell therapy is a special treatment for some blood cancers. To get this therapy, you must meet certain criteria. This includes the type and stage of your cancer, your past treatments, and your overall health.
If you haven’t gotten better with usual treatments like chemo or radiation, you might be eligible. Talking to your doctor and a cancer center that offers CAR T-cell therapy is key. These places have the right team and setup to handle the treatment and any side effects.
There are CAR T-cell therapy centers all over the U.S. Your doctor can help find one near you and guide you through the process.
But, CAR T-cell therapy isn’t available everywhere yet. Making CAR T-cells takes time, and centers can only treat a few patients at once. As research grows and more centers start using this therapy, more people will have access to it. This brings hope to those fighting blood cancers.
FAQ
Q: What is CAR T-cell therapy?
A: CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. This is done by changing T-cells to recognize and destroy cancer.
Q: How does the CAR T-cell therapy process work?
A: The process starts with checking the patient’s health. Then, T-cells are collected. Next, these cells are changed to fight cancer.
After that, the patient gets chemotherapy to prepare their body. The changed T-cells are then given to the patient. The patient is closely watched after treatment.
Q: What types of cancer can CAR T-cell therapy treat?
A: CAR T-cell therapy is approved for some blood cancers. These include acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). Researchers are also looking into treating other cancers.
Q: What are the possible side effects of CAR T-cell therapy?
A: Side effects can include cytokine release syndrome (CRS) and neurotoxicity. Other side effects may happen. Doctors watch patients closely to manage these issues.
Q: How long does the CAR T-cell therapy process take?
A: The whole process can take weeks to months. It depends on the patient’s case and how long it takes to make the CAR T-cells.
Q: Who is eligible for CAR T-cell therapy?
A: Who can get CAR T-cell therapy depends on their cancer type and health. Patients should talk to their doctor to see if it’s right for them.
Q: How can I access CAR T-cell therapy?
A: You can get CAR T-cell therapy at special cancer centers in the U.S. You need a doctor’s referral. It’s important to talk to your doctor about this option.
Q: What is the success rate of CAR T-cell therapy?
A: Success rates vary based on the cancer and the patient. Some patients have seen complete remission. But, results can differ, and more data is needed.
Q: Is CAR T-cell therapy a one-time treatment?
A: Usually, CAR T-cell therapy is given once. The T-cells can keep fighting cancer for a long time. But, some patients might need more treatment.
Q: What is the cost of CAR T-cell therapy?
A: CAR T-cell therapy is expensive. The cost depends on the treatment and insurance. Patients should talk to their doctor and insurance about the cost.
Q: Are there any long-term side effects of CAR T-cell therapy?
A: Long-term effects are not fully known yet. Patients are watched for any long-term problems. Researchers are studying the long-term effects of this treatment.
Q: Can CAR T-cell therapy be used in combination with other cancer treatments?
A: Right now, CAR T-cell therapy is used alone for some blood cancers. But, research is looking into using it with other treatments. This could make it more effective for more cancers.


















