Millions of people live with chronic conditions, and knowing what is type 1 diabetes mellitus is key. This disease is caused by the body attacking itself, making it hard to use glucose. It brings many health problems, both short and long term.
For those with type 1 diabetes, managing it is a big job. It needs constant care, knowing a lot about the disease, and being aware of type 1 diabetes complications.
People with type 1 diabetes have to keep learning and adjusting. Learning about the disease early helps control it better. This helps avoid many problems that come from not managing it well. This guide is the start of understanding type 1 diabetes mellitus and how to manage it every day.
What is Type 1 Diabetes Mellitus
Type 1 Diabetes Mellitus (T1DM) is an autoimmune disease. It makes the pancreas unable to make enough insulin. This results in high blood sugar levels, which need daily insulin for type 1 diabetes treatment. Knowing the type 1 diabetes causes helps in early diagnosis and treatment.
Insulin therapy is key in type 1 diabetes treatment. Without it, people with T1DM face serious health issues. Treatment includes lifestyle changes and ongoing medical care.
| Treatment | Purpose | Frequency |
|---|---|---|
| Daily Insulin Injections | To regulate blood glucose levels | Multiple times a day |
| Continuous Glucose Monitoring (CGM) | Real-time glucose level tracking | Continuous |
| Diet Adjustments | Stabilize and optimize blood sugar | Daily |
To manage hair loss due to diabetes, controlling blood sugar is key. Understanding the hormonal effects is also important. More on this can be found at understanding the connection between diabetes and hair.
The Onset of Type 1 Diabetes: Recognizing Early Symptoms
Type 1 diabetes can start quickly and quietly. It’s key to spot the signs early. This helps get medical help fast and avoid serious problems.
Common Early Symptoms of Type 1 Diabetes
Symptoms of type 1 diabetes can appear fast and get worse quickly. Here are the main signs:
- Excessive thirst – Often unquenchable, leading to a significant increase in water consumption.
- Frequent urination – An unusually high need to urinate, often disrupting normal daily activities and sleep patterns.
- Unexplained weight loss – Rapid weight loss despite no change in diet or exercise routine.
- Increased hunger – Persistent hunger even after eating, caused by the body’s inability to utilize glucose effectively.
- Blurry vision – A sudden occurrence of blurred vision not linked to any known eye conditions.
- Fatigue – Feeling unusually tired or lethargic without adequate reason.
The Critical Nature of Early Detection
Spotting type 1 diabetes symptoms early and getting medical help fast is key. This leads to a quick type 1 diabetes diagnosis. Early detection is vital for managing the disease well and avoiding serious complications.
Doctors use different tests to confirm a diagnosis and start treatment. These tests are important for finding the best way to manage the condition and keep a good quality of life.
Thanks to medical progress, managing type 1 diabetes early is easier. Tools like Continuous Glucose Monitors (CGMs) and custom insulin plans can make a big difference. This shows how important it is to catch the disease early and accurately.
Exploring the Immunological Causes of Type 1 Diabetes
Type 1 diabetes is caused by the body’s immune system attacking and destroying insulin-making cells in the pancreas. This attack is a key reason why managing type 1 diabetes is so important.
Learning how to manage type 1 diabetes well is key to improving life for those with it. Finding out what triggers this immune response is vital for creating better treatments.
Looking deeper into how the immune system works can help. This is explored in this detailed article on immuno-related research.
| Factor | Description | Impact |
|---|---|---|
| Autoantibodies | Immune proteins that mistakenly attack body’s own cells | Direct destruction of beta cells |
| Genetic predisposition | Hereditary factors that influence immune system characteristics | Increases susceptibility to immune system dysregulation |
| Environmental triggers | Exposure to certain viruses and toxins | Potential initiation of autoimmunity |
To better manage type 1 diabetes, it’s important to understand and control these immune factors. Staying up-to-date with research and new medical findings is essential in fighting the root causes of type 1 diabetes.
Understanding the Role of Genetics in Type 1 Diabetes
Genetics play a big role in type 1 diabetes. They can affect how likely someone is to get type 1 diabetes complications. This part talks about the important genetic factors and family patterns in this autoimmune disease.
The Genetic Risk Factors
Studies have found several genes linked to type 1 diabetes. The HLA complex is key. It helps the immune system tell self from non-self. Changes in this gene group raise the risk of type 1 diabetes.
Family History and Hereditary Patterns
Type 1 diabetes often runs in families. It’s due to many genes working together. If a family member has it, your risk goes up. Knowing your family history can help spot risks early and prevent severe problems.
| Relationship | Risk Increase |
|---|---|
| Parent with Type 1 Diabetes | Approximately 6% |
| Sibling with Type 1 Diabetes | Approximately 5% |
Knowing your genes and family history can lead to early detection. This gives a chance to stop or slow type 1 diabetes complications. More research and genetic tests aim to find treatments that fit each person’s genes.
Type 1 Diabetes Diagnosis: Methods and Criteria
The journey to a type 1 diabetes diagnosis starts with noticing symptoms. These include being very thirsty, needing to pee a lot, and losing weight without trying. Spotting these signs early is key to managing the disease well.
To accurately diagnose type 1 diabetes, doctors use blood tests. These tests check glucose levels and look for autoantibodies. Here’s a table showing the main tests and what they check:
| Test | Description | Necessary Criteria for Diagnosis |
|---|---|---|
| Glycated Hemoglobin (A1C) Test | This test shows your blood sugar level over two to three months. | An A1C level of 6.5% or higher on two tests means diabetes. |
| Random Blood Sugar Test | This test takes a blood sample at any time, not after eating. | A blood sugar level of 200 mg/dL or higher suggests diabetes. |
| Fasting Blood Sugar Test | This test checks blood sugar after not eating for a night. | A fasting blood sugar level of 126 mg/dL or higher on two tests means diabetes. |
| Autoantibody Tests | These tests look for specific antibodies in type 1 diabetes. | Finding one or more autoantibodies is a strong sign of type 1 diabetes. |
It’s not just doctors who need to know the symptoms of type 1 diabetes. Patients and their families should also be aware. This way, they can get help quickly. Early treatment helps manage the disease better and prevents serious problems.
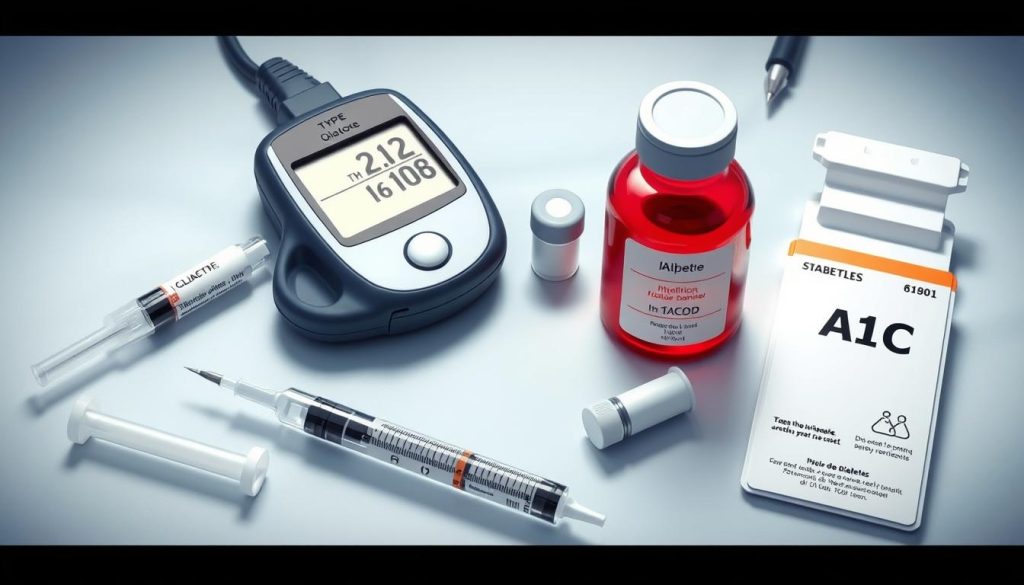
In short, a type 1 diabetes diagnosis comes from checking symptoms and doing blood tests. This careful method helps doctors diagnose accurately. Knowing about symptoms and the testing process is important for those at risk of type 1 diabetes.
Comparing Type 1 and Type 2 Diabetes: Key Differences
It’s important to know the differences between type 1 and type 2 diabetes. Both affect how the body handles blood sugar. But, they have different causes and treatments.
Pathophysiology of Type 1 vs. Type 2
Type 1 diabetes is an autoimmune disease. It happens when the immune system attacks insulin-making cells in the pancreas. Type 2 diabetes, on the other hand, is about insulin resistance. This means the body’s cells don’t use insulin well, and the pancreas makes less insulin over time.
Symptom Comparison
Type 1 diabetes shows up quickly and often in younger people. Symptoms include being very thirsty, needing to pee a lot, and losing weight without trying. Type 2 diabetes symptoms come on slower. They might include feeling tired and seeing things less clearly.
Treatment Approaches
For type 1 diabetes, taking insulin every day is key. People with this condition don’t make much insulin. Type 2 diabetes treatment starts with diet and exercise. If that doesn’t work, doctors might prescribe medication or insulin.
Doctors tailor treatments to each patient. Research is always looking for better ways to treat type 1 diabetes.
| Type 1 Diabetes | Type 2 Diabetes | |
|---|---|---|
| Primary Cause | Autoimmune destruction of insulin-producing cells | Insulin resistance followed by insulin deficiency |
| Common Onset | Childhood/Adolescence | Adult, increasing with age |
| Key Treatment | Insulin injections/Insulin pump | Diet, exercise, oral medications, possibly insulin |
Personalizing Management Strategies for Type 1 Diabetes
Managing type 1 diabetes well needs a personal touch, mainly in what you eat and how much you move. Making these choices your own can really improve your life and control over the disease.
Custom Diet Plans for Insulin Regulation
It’s key to have a diet plan for type 1 diabetes that fits you. Everyone reacts differently to food, so it’s all about finding what works for you. Talking to a dietitian can help make a meal plan that fits your food likes and lifestyle, helping with insulin control.
- Integration of low glycemic index foods to stabilize blood sugar
- Balanced intake of proteins, fats, and fibers to support overall health
- Portion control to prevent blood sugar spikes
Changing your diet in these ways is key to managing type 1 diabetes well and staying healthy.
Importance of Regular Exercise
Exercise is also a big part of managing type 1 diabetes. It makes your body better at using insulin, helping control blood sugar. It also helps keep your weight healthy, which lowers the chance of other health problems.
- Aerobic exercises such as walking, swimming, and cycling
- Resistance training to build muscle mass and increase metabolism
- Flexibility exercises to maintain muscle elasticity and joint health
Staying active regularly can really help manage type 1 diabetes better, making you feel better and more in control.
In short, custom diets and regular exercise are vital for managing type 1 diabetes. These should be made to fit your needs to avoid common problems, leading to a more active and balanced life.
Administering and Adjusting Insulin for Type 1 Diabetes
Managing type 1 diabetes well means using insulin in a way that fits each person’s needs. It’s important to know about the different types of insulin and how they work. This helps make treatment better for each person.
Different Types of Insulin Therapies
There are many types of insulin for type 1 diabetes, each with its own benefits. They depend on when and how much insulin a person needs. Here are a few:
- Rapid-acting insulin: Starts working fast, within 15 minutes. It’s best for controlling blood sugar after meals.
- Long-acting insulin: Keeps blood sugar stable all day and night. It doesn’t have a big peak.
- Premixed insulin: Mixes rapid-acting and intermediate-acting insulin. It makes things simpler for some people.
Insulin Dosage and Administration Techniques
Finding the right amount of insulin and how to take it is tricky. It depends on the person’s lifestyle, blood sugar patterns, and how they react to insulin.
- Subcutaneous injections: This is the most common way, using syringes, pens, or pumps.
- Insulin pumps: These small devices on the body give insulin all the time.
- Inhaled insulin: A quick-acting type that goes into the lungs. It’s for those who don’t like injections.
| Insulin Type | Onset | Peak | Duration |
|---|---|---|---|
| Rapid-acting | 15-30 min | 1-2 hrs | 3-5 hrs |
| Long-acting | 1 hr | No pronounced peak | Up to 24 hrs |
| Premixed | 30 min | 2-4 hrs | 16-24 hrs |
To get the most out of insulin for type 1 diabetes, you need to balance your lifestyle and keep a close eye on your blood sugar. This tailored approach is key to good type 1 diabetes treatment.
Blood Glucose Monitoring and Target Levels
For those with type 1 diabetes, keeping blood glucose levels in check is key. Regular checks help make smart choices about what to eat, how much to exercise, and how much insulin to take. This part talks about how to track glucose levels and set realistic goals.
Good management begins with a correct type 1 diabetes diagnosis. After that, checking blood glucose becomes a daily routine. There are different devices for this, from simple glucometers to continuous glucose monitors (CGM). CGMs show real-time data and trends.
- Glucometers are small, simple to use, and need just a tiny blood sample.
- Continuous Glucose Monitors track glucose all day without needing to prick your finger many times.
It’s also vital to know your target glucose levels. These levels help shape your management plan. They can change based on your health, lifestyle, and doctor’s advice.
| Time of day | Target Blood Glucose Levels (mg/dL) |
|---|---|
| Before meals | 70-130 |
| 1-2 hours after beginning of the meal | Less than 180 |
| Bedtime | 100-140 |
Changing these targets might be needed based on your ongoing checks and doctor’s advice. Keeping your goals up to date is key to managing type 1 diabetes well.
Navigating Challenges in Living with Type 1 Diabetes
Living with type 1 diabetes is more than just managing blood sugar and insulin. It also affects your mental and social health. These challenges can change how you interact with others and how you feel about yourself.

Mental Health and Emotional Well-being
People with type 1 diabetes often feel anxious about their condition. They worry about their blood sugar levels and the risks of type 1 diabetes complications. This worry can make managing their diabetes even harder.
It’s important to take care of your mental health. Counseling and therapy can help improve your life quality. Mindfulness practices, like meditation, can also help manage stress and keep blood sugar levels stable.
Support Systems and Communities
Having a strong support system is key for those with type 1 diabetes. Family, friends, healthcare providers, and community groups offer both emotional and practical help.
- Family and friends provide daily support and understanding, essential for long-term management.
- Healthcare teams offer medical guidance and emotional support tailored to your needs.
- Online and local diabetes communities offer a place to share experiences and find encouragement, helping to combat feelings of loneliness.
This network is vital for managing diabetes. It helps reduce the daily stress of diabetes care, making it easier to handle type 1 diabetes complications with confidence and determination.
Avoiding and Managing Type 1 Diabetes Complications
Managing type 1 diabetes well can lower the risk of serious type 1 diabetes complications. These include heart disease, kidney damage, and nerve damage. Taking proactive steps can prevent these issues and improve life quality for those with type 1 diabetes.
To manage type 1 diabetes, it’s important to check blood sugar often, eat right, and stay active. Also, yearly health checks are key to catch and treat heart, kidney, and nerve problems early.
| Complication | Description | Preventive Measures |
|---|---|---|
| Cardiovascular Disease | Increased risk of heart disease and stroke. | Regular exercise, dietary adjustments, medication as prescribed. |
| Nephropathy | Kidney damage leading to reduced function or failure. | Control blood sugar, blood pressure, annual kidney function tests. |
| Neuropathy | Deterioration of nerve functions, specially in extremities. | Maintain blood sugar levels, foot care, regular check-ups. |
Every person with type 1 diabetes is different. That’s why making a treatment plan that fits them is so important. Working with doctors to create a diabetes management plan can really help avoid type 1 diabetes complications.
Advancements in Type 1 Diabetes Treatment Options
The world of type 1 diabetes treatment is changing fast. New ideas in insulin delivery and fixing damaged cells are making a big difference. These changes aim to make life better for those with this condition.
Breakthroughs in Insulin Delivery Systems
New tech has made managing insulin for type 1 diabetes easier. One big step is combining Continuous Glucose Monitors (CGMs) with insulin pumps. This creates a closed-loop system, or artificial pancreas, that adjusts insulin automatically.
This system helps keep blood sugar levels stable. It makes managing diabetes less of a hassle for patients.
- Increased accuracy in insulin dosing
- Reduced incidence of hypo- and hyperglycemia
- Improved quality of life for users
These advancements are a big step forward in diabetes care. They offer a smoother, less invasive way to manage the condition.
Emerging Research on Beta Cell Replacement
Research on beta cell replacement is also exciting. Scientists are working on protecting or replacing lost beta cells with stem cells. This could change how we treat type 1 diabetes, moving from symptom management to a possible cure.
Recent studies have shown lab-grown beta cells that work like natural ones. This is a big step towards a future where insulin injections might not be needed.
As research in type 1 diabetes moves forward, the goal is to make daily management easier. This could lead to better health and a better life for patients. With more research and investment, the future of type 1 diabetes treatment looks bright and could even lead to a cure.
The Impact of Dietary Choices on Type 1 Diabetes
Learning about the type 1 diabetes diet is key to keeping blood sugar stable. Making smart food choices can greatly help manage type 1 diabetes. This way, people can live a healthier, more balanced life.
Carbohydrate Counting and Meal Planning
Carbohydrate counting is essential for type 1 diabetes management. It tracks carbs in meals and snacks, affecting blood sugar. Knowing how to count carbs helps adjust insulin doses for better glucose control.
Planning meals with carb awareness offers more control over the type 1 diabetes diet. It helps avoid blood sugar spikes and drops. It also ensures a balanced diet, meeting all nutritional needs.
Glycemic Index and Type 1 Diabetes Management
The Glycemic Index (GI) shows how fast foods raise blood sugar. Foods with a low GI digest slowly, causing a gradual blood sugar increase. This makes managing type 1 diabetes easier. Choosing foods based on GI can help control blood sugar levels after meals.
| Food Category | Low GI Foods | High GI Foods |
|---|---|---|
| Fruits | Apples, Berries | Pineapple, Watermelon |
| Vegetables | Carrots, Broccoli | Potatoes, Corn |
| Grains | Whole Wheat Bread, Brown Rice | White Bread, White Rice |
| Dairy | Yogurt, Milk | Ice Cream, Soft Cheese |
By choosing low GI foods and mastering carbohydrate counting, people with type 1 diabetes can improve their diet management. This leads to more stable blood glucose levels.
Exercise Considerations for Individuals with Type 1 Diabetes
For those with type 1 diabetes, adding regular exercise to their routine is key. But, it’s important to plan carefully to keep blood sugar levels stable. This section will cover essential tips for safely exercising with type 1 diabetes.
First, it’s critical to check blood sugar before, during, and after working out. Exercise lowers blood sugar, and each activity affects it differently. Testing blood sugar more often and adjusting insulin doses on active days can help avoid low blood sugar.
- Type of exercise – Cardio and strength training need different glucose management plans.
- Duration and intensity – Longer or more intense workouts can lower blood sugar for longer.
- Timing of insulin – Adjusting insulin timing with exercise can help control blood sugar.
Stable blood sugar levels also depend on the right snacks or meals before and after exercise. Eating carbs may be needed to prevent low blood sugar, mainly in long or intense workouts.
| Activity Type | Carbohydrate Strategy | Insulin Adjustment |
|---|---|---|
| Light Cardio | Small carb snack | Minor or no change |
| Intense Cardio | Larger carb intake | Significant decrease |
| Strength Training | Moderate carbs | Depends on intensity |
Also, the time of day for exercise matters. Morning workouts might affect insulin sensitivity differently than evening ones. It’s best to watch how your body reacts and create a workout plan that fits your diabetes management.
Educational Resources and Support for Type 1 Diabetics
Learning about type 1 diabetes (T1DM) is key for those living with it. There are many type 1 diabetes educational resources out there. The American Diabetes Association (ADA) has a wealth of materials to help understand and manage T1DM.
They offer tips on diet, exercise, and how to take medication. These are vital for daily life with T1DM.
Online groups like the T1D Exchange are also great. They let people share their stories, get advice, and find friends. The Diabetes Education and Camping Association (DECA) runs programs for kids. They learn about diabetes while having fun, which helps them manage their condition better.
It’s important for patients, caregivers, and families to have access to these type 1 diabetes educational resources. Organizations like the JDRF’s Bag of Hope and the College Diabetes Network help at every stage of life. They make sure support is there, no matter the age or situation.
By spreading awareness and education, we aim to improve the lives of those with type 1 diabetes. Our goal is to enhance care and support for them.
FAQ
Q: What is Type 1 Diabetes Mellitus?
A: Type 1 Diabetes Mellitus (T1DM) is an autoimmune disease. It happens when the pancreas doesn’t make enough insulin. Insulin is key for controlling blood sugar. People with T1DM need to take insulin for life, check their blood sugar often, and follow a special diet and exercise plan.
Q: How is Type 1 Diabetes different from Type 2?
A: Type 1 Diabetes is when the immune system attacks insulin-making cells. Type 2 Diabetes is when the body doesn’t use insulin well. T1DM always needs insulin, but T2DM might be managed with diet and medication first.
Q: What are the early symptoms of Type 1 Diabetes?
A: Early signs of Type 1 Diabetes include being very thirsty, needing to pee a lot, feeling hungry all the time, being tired, seeing things blurry, and losing weight without trying. Spotting these signs early is key for getting the right treatment.
Q: What causes Type 1 Diabetes?
A: The exact reason for T1DM is not fully understood. It’s thought to be a mix of genes and something in the environment that makes the immune system attack insulin-making cells in the pancreas.
Q: Can Type 1 Diabetes be genetically inherited?
A: Type 1 Diabetes isn’t passed down directly. But having a family member with it raises your risk. Genes play a part, but something in the environment also triggers it.
Q: How is Type 1 Diabetes diagnosed?
A: Doctors use blood tests to find T1DM. These include the A1C test, which shows blood sugar levels over three months, glucose tolerance tests, and tests for autoantibodies found in T1DM.
Q: What is involved in the treatment of Type 1 Diabetes?
A: T1DM treatment focuses on keeping blood sugar in check. This includes insulin therapy, like injections or an insulin pump, eating right, exercising regularly, and checking blood sugar often.
Q: Can people with Type 1 Diabetes lead a normal life?
A: Yes, with the right care, people with Type 1 Diabetes can live a normal life. They need to manage their blood sugar, eat well, exercise, and see their doctor regularly to avoid complications.
Q: What are the most common complications of Type 1 Diabetes?
A: Common complications of T1DM include heart disease, nerve damage, kidney damage, eye damage, and a higher risk of infections. Keeping blood sugar levels stable can help prevent these problems.
Q: How does diet affect Type 1 Diabetes management?
A: Diet is very important for managing T1DM. Counting carbs and knowing the glycemic index helps choose foods that keep blood sugar stable. A balanced diet also helps overall health.
Q: What new treatments for Type 1 Diabetes are being researched?
A: New treatments include advanced insulin delivery systems and devices like the artificial pancreas. Researchers are also looking into beta cell replacement therapy and immunotherapy to change how T1DM is treated.
Q: How important is exercise for someone with Type 1 Diabetes?
A: Exercise is very important for T1DM management. It makes the body more sensitive to insulin and helps keep blood sugar in range. But, it’s important to watch blood sugar closely and adjust insulin doses when exercising.
Q: What resources are available for individuals with Type 1 Diabetes?
A: There are many resources for T1DM, like diabetes education programs, support groups, non-profit organizations, and online communities. They offer information, support, and a community for people with T1DM and their families.