Colon resection surgery is key in treating many gut problems. This guide will cover the surgery, recovery, and what to expect. It’s for those thinking about or getting ready for this surgery.
Learning about colon resection surgery helps patients make smart health choices. It talks about getting ready for surgery and recovering afterwards. It’s packed with important info for those going through this big medical step.
Knowing about colon resection surgery helps patients get ready for treatment and healing. This knowledge helps set realistic goals and makes recovery easier. It leads to better surgery results and a better life.
Understanding Colon Resection Surgery
Colon resection surgery, also known as colorectal surgery or colectomy, removes part or all of the colon. It’s key for treating many intestinal issues and boosting patients’ quality of life.
Definition and Medical Terminology
A colectomy is when doctors surgically take out a part of the large intestine. It’s also called a bowel resection or large bowel resection. How much is removed depends on the condition being treated.
Types of Colectomy Procedures
There are several colectomy procedures, each targeting different parts of the colon:
- Total colectomy: Removal of the entire colon
- Partial colectomy: Removal of a specific section of the colon
- Hemicolectomy: Removal of either the right or left side of the colon
Common Reasons for Surgery
Colorectal surgery is needed for many reasons:
- Colon cancer
- Diverticulitis
- Inflammatory bowel diseases (e.g., Crohn’s disease, ulcerative colitis)
- Bowel obstruction
- Severe gastrointestinal bleeding
Knowing about colon resection surgery helps patients get ready for it and understand recovery. Your doctor will tell you which colectomy you need based on your condition and health.
Medical Conditions Requiring Bowel Surgery
Bowel surgery is needed for many medical conditions. It includes intestinal resection and abdominal surgery. These procedures treat severe digestive problems that other treatments can’t fix.
Colon cancer often needs surgery. Doctors remove tumors in the large intestine. This stops cancer from spreading and helps patients get better.
Inflammatory bowel diseases like Crohn’s and ulcerative colitis may need surgery. These diseases cause inflammation, ulcers, and damage to the digestive tract. Surgery is needed when medicine doesn’t work.
Diverticulitis, where small pouches in the colon get inflamed or infected, might need surgery. Severe cases or repeated problems often require removing the affected colon part.
Bowel obstructions are another reason for surgery. These blockages can come from scar tissue, hernias, or tumors. Surgery aims to remove the blockage and fix bowel function.
| Condition | Surgical Approach | Recovery Time |
|---|---|---|
| Colon Cancer | Partial or total colectomy | 4-6 weeks |
| Crohn’s Disease | Bowel resection | 3-6 weeks |
| Ulcerative Colitis | Total colectomy with ileostomy | 6-8 weeks |
| Diverticulitis | Sigmoid colectomy | 2-4 weeks |
| Bowel Obstruction | Lysis of adhesions or resection | 1-3 weeks |
Getting surgery on time can prevent serious problems and improve life quality. It’s important to talk to a healthcare provider to find the best treatment.
Pre-operative Preparation and Assessment
Getting ready for gastrointestinal surgery is key. Your healthcare team will help you every step of the way. They want to make sure your digestive surgery goes well.
Medical Evaluation Requirements
You’ll have to go through several tests before surgery. These might include blood work, imaging studies, and a colonoscopy. These tests help your team plan your care and reduce risks.
| Evaluation Type | Purpose |
|---|---|
| Blood Tests | Check overall health and infection markers |
| Imaging Studies | Visualize the affected area of the colon |
| Colonoscopy | Examine the entire colon for abnormalities |
Dietary Restrictions Before Surgery
Your doctor will tell you what to eat and drink before surgery. You might need to stick to a clear liquid diet or do bowel prep to clean your intestines.
Medication Adjustments
Some medicines might need to be stopped or changed before surgery. Tell your surgeon about all your medications, including over-the-counter drugs and supplements.
- Blood thinners may need to be stopped
- Diabetes medications might require adjustment
- Certain supplements should be avoided

By following these guidelines, you can make your surgery and recovery smoother.
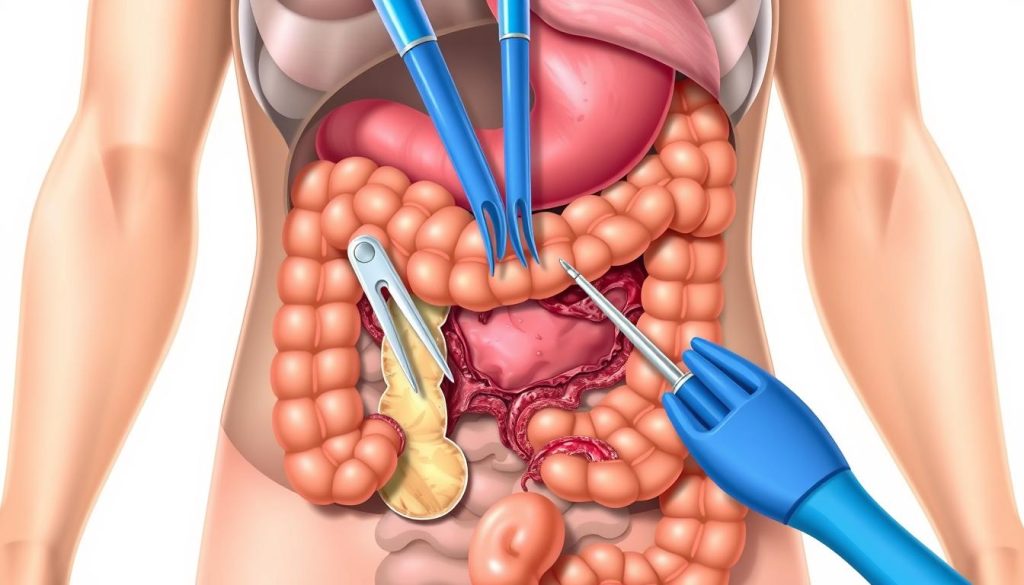
Surgical Techniques and Approaches
Colon resection surgery has seen big improvements in surgical oncology. Now, surgeons have many techniques to choose from. Each method has its own benefits and things to think about for patients.
Open Surgery Method
Open surgery means a big cut in the belly. It’s a traditional way that lets surgeons see the colon directly. It’s good for complicated cases or when they need to explore a lot. But, it takes longer to recover from.
Laparoscopic Procedure
Laparoscopic surgery uses small cuts and special tools. A camera helps the surgeon see what they’re doing. It’s less invasive, leading to quicker recovery and less pain. It’s popular for many patients.
Robotic-Assisted Surgery
Robotic surgery combines technology with a surgeon’s skills. The surgeon uses robotic arms for precise work. It’s great for complex cases where accuracy is key.
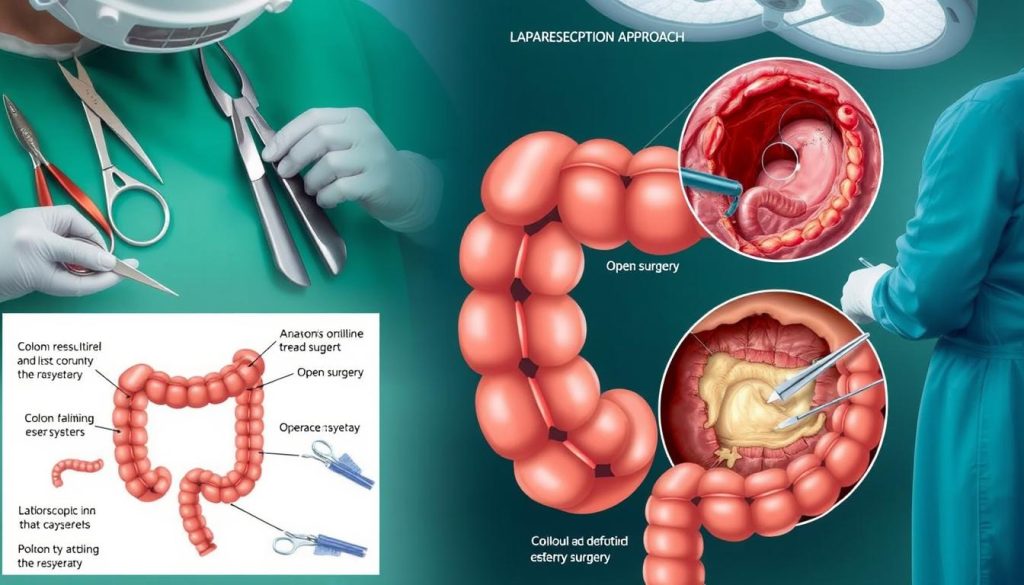
| Technique | Incision Size | Recovery Time | Best For |
|---|---|---|---|
| Open Surgery | Large (6-8 inches) | 4-6 weeks | Complex cases |
| Laparoscopic | Small (0.5-1 inch) | 2-3 weeks | Most standard cases |
| Robotic-Assisted | Small (0.5-1 inch) | 2-3 weeks | Precision-demanding cases |
The right surgery depends on many things like where the tumor is, the patient’s health, and the surgeon’s skills. Talking to your healthcare team helps pick the best surgery for you.
Step-by-Step Colon Resection Surgery Procedure
Colon resection surgery is a precise process. It starts with the patient under general anesthesia. Surgeons then make an incision in the abdomen, either traditionally or through minimally invasive methods.
Next, the team finds the affected colon part. They carefully separate it from nearby tissues, managing blood vessels well. The diseased segment is removed, and the healthy ends are joined together.
This joining, called anastomosis, is key. Surgeons use stapling devices or sutures for a secure seal. They check for leaks to avoid complications. Sometimes, a temporary colostomy is needed.
During surgery, the team watches vital signs and makes adjustments. The whole process can take several hours, based on the case’s complexity. Afterward, the incision is closed with sutures or staples.
Knowing this can make patients feel more comfortable about their surgery. It shows how far medical science has come in treating colon issues.
Anesthesia and Operating Room Preparation
Getting ready for a colectomy or intestinal resection needs careful planning. The setup of the anesthesia and operating room is key to a successful surgery.
Types of Anesthesia Used
General anesthesia is the top choice for colectomy surgeries. It keeps the patient asleep and pain-free. Sometimes, regional anesthesia and sedation are used for specific intestinal resection methods.
Monitoring During Surgery
The surgical team watches vital signs closely during the colectomy. They check heart rate, blood pressure, oxygen levels, and body temperature. Advanced tools help keep the patient safe during the surgery.
Surgical Team Roles
A well-trained team works together for a colectomy. The surgeon does the surgery and the intestinal resection. An anesthesiologist handles pain and watches the patient’s vital signs. Surgical assistants and nurses help by handing tools and keeping the area clean.
| Team Member | Primary Responsibilities |
|---|---|
| Surgeon | Performs colectomy, directs surgical approach |
| Anesthesiologist | Administers anesthesia, monitors patient vitals |
| Surgical Assistant | Aids surgeon, manages surgical tools |
| Scrub Nurse | Ensures sterile field, hands instruments to surgeon |
| Circulating Nurse | Manages operating room, documents procedure |
This teamwork makes sure every part of the colectomy is done with care. It starts with the anesthesia and ends with the final steps of the surgery.
Potential Risks and Complications
Colon resection surgery, like any major surgery, has risks. It’s important for patients to know these before surgery. Knowing the risks helps in making informed decisions and setting realistic expectations.
- Infection at the surgical site
- Bleeding during or after surgery
- Anastomotic leak (separation of the newly connected bowel sections)
- Bowel obstruction
- Changes in bowel habits
Surgeons take steps to lower these risks. They use clean techniques, watch for blood loss, and make sure bowel segments connect well. Even with these precautions, complications can happen.
Following post-operative instructions is key to reducing risks. Proper wound care and sticking to dietary restrictions can help a lot. For more information, check out proper wound care guidelines.
| Complication | Frequency | Prevention Measures |
|---|---|---|
| Surgical site infection | 5-10% | Antibiotics, sterile technique |
| Anastomotic leak | 1-3% | Careful suturing, nutrition support |
| Bowel obstruction | 2-5% | Early mobilization, proper diet |
Even with risks, most patients do well after colon resection surgery. With the right care and follow-up, surgeons and medical teams can manage any complications. This ensures the best outcomes for patients going through this important surgery.
Immediate Post-operative Care
After digestive surgery, patients start a critical recovery phase. The care in the hours after surgery is key for a good outcome. This time is filled with close monitoring and careful management to help healing begin well.
Recovery Room Monitoring
Nurses watch over patients in the recovery room. They check vital signs like heart rate, blood pressure, and oxygen levels often. The surgical site is checked for bleeding or infection signs. Patients may feel drowsy as they wake up, but nurses are there to comfort and reassure them.
Pain Management Protocols
Managing pain is a major focus after surgery. Doctors use different methods to keep patients comfortable:
- Intravenous pain medications
- Epidural analgesia for extended relief
- Patient-controlled analgesia pumps
These options help tailor pain management to each patient. This way, patients can rest and start healing.
Initial Mobility Guidelines
Moving early is important for recovery. Nurses guide patients to:
- Take deep breaths and cough to prevent lung issues
- Move their legs to improve circulation
- Sit up and eventually walk short distances
These simple steps can help recovery speed up and lower the risk of complications after surgery.
Hospital Recovery Period
After colon resection surgery, patients usually stay in the hospital for a few days. This time is key for doctors to watch over them and handle any issues. How long you stay depends on the surgery type and how fast you heal.
Right after surgery, patients start moving from IV fluids to eating. They begin with clear liquids and then soft foods. This helps the colon heal without too much stress.
Looking after the wound is very important. Nurses clean and check the surgery area often. They teach patients how to care for it at home. Drains might be used to remove extra fluids, and removing them is a big step in getting better.
Getting up and moving is a slow but important step. Patients are told to do deep breathing and coughing gently. As they get stronger, they can walk more around the hospital.
“Recovery from colon resection surgery is a journey. Each day brings new challenges and victories as patients work towards regaining their health and independence.”
Having someone to support you emotionally is also key. Hospital staff offer encouragement and help with both the physical and emotional sides of healing. Before leaving, patients get clear instructions for their recovery at home. This helps them smoothly move into the next part of their healing journey.
Long-term Recovery and Rehabilitation
Recovery from colorectal surgery is more than just leaving the hospital. Patients who have a colectomy start a long journey. They work on getting stronger, adjusting to new diets, and slowly getting back to their daily routines.
Physical Activity Guidelines
Patients should begin with light movements after a colectomy. Walking is important in the beginning. As they get stronger, they can do more.
Most people can go back to work in 4-6 weeks. But, they should avoid heavy lifting for 6-8 weeks. Always check with your surgeon before starting any exercise.
Dietary Modifications
Diet is very important during recovery. Start with clear liquids and then move to soft foods. Slowly add solid foods as you can handle them.
Avoid foods high in fiber at first. Eat small meals often to help with digestion. Drinking plenty of water is also key. Your doctor might suggest nutritional supplements.
Follow-up Care Schedule
Regular doctor visits are essential after a colectomy. Here’s what you can expect:
- First visit: 1-2 weeks after surgery
- Second visit: 4-6 weeks after surgery
- Subsequent visits: Every 3-6 months for the first two years
These visits help check on your healing, answer questions, and watch for any problems. Recovery from colorectal surgery takes time and effort. But, with the right care and following the guidelines, most people can get back to their lives.
Lifestyle Changes After Colorectal Surgery
Having intestinal resection or abdominal surgery can change your life a lot. You might notice changes in your daily habits and how you go to the bathroom. You’ll need to find new ways to handle these changes.
After surgery, your digestive system might act differently. You might go to the bathroom more often or have trouble with constipation. Getting used to these changes takes time and effort.
Emotional and psychological effects are common after colorectal surgery. Some people worry about how they look or feel nervous in social situations. It’s important to talk about these feelings and get help when you need it.
- Adjust your diet to accommodate new digestive patterns
- Stay hydrated to support healthy bowel function
- Engage in gentle exercise as approved by your doctor
- Join support groups to connect with others who’ve had similar experiences
Intimate relationships can also be affected after surgery. Talking openly with your partner is important. With time and patience, you can get back to normal activities and relationships.
| Area of Change | Potential Impact | Coping Strategy |
|---|---|---|
| Diet | Altered digestion | Gradual food reintroduction |
| Physical Activity | Limited mobility | Tailored exercise plan |
| Social Life | Anxiety about outings | Start with short, planned trips |
Remember, adjusting to life after surgery takes time. Be kind to yourself and don’t be afraid to ask for help. Your healthcare providers are there to guide and support you during your recovery.
Nutrition and Diet Recommendations
After gastrointestinal surgery, eating right is key to getting better. Patients need to watch what they eat to help their bodies heal and avoid problems.
Foods to Avoid
In the first few days, stay away from foods that might upset your stomach or slow healing. These include:
- High-fiber foods like raw vegetables and whole grains
- Spicy or heavily seasoned dishes
- Fatty or fried foods
- Carbonated beverages
- Alcohol
Recommended Dietary Changes
To help your body heal, eat foods that are easy to digest and full of nutrients:
- Lean proteins such as chicken, fish, and tofu
- Cooked vegetables
- Low-fat dairy products
- Soft fruits like bananas and melons
- Smoothies and protein shakes
Supplement Considerations
Some supplements might help you recover from gastrointestinal surgery. Talk to your doctor about:
- Multivitamins to address possible nutrient gaps
- Probiotics to boost gut health
- Iron supplements if you’re at risk for anemia
- Vitamin B12, if you had part of your small intestine removed
Keep in mind, everyone’s nutritional needs are different. Work with your healthcare team to create a diet plan that’s right for you after digestive surgery.
Physical Activity and Exercise Guidelines
After colon resection surgery, it’s important to start moving again slowly. Patients need to follow certain rules to heal right and avoid problems.
Begin with easy steps like short walks around your house. As you get stronger, walk further and longer. This helps avoid blood clots and boosts blood flow.
Don’t lift heavy things or do hard activities for 6-8 weeks after surgery. Your doctor will tell you when it’s okay to go back to work, drive, and do harder exercises. This depends on how well you’re recovering.
- Week 1-2: Focus on walking and light stretching
- Week 3-4: Gradually increase walking distance and add gentle yoga
- Week 5-6: Introduce low-impact exercises like swimming or stationary cycling
- Week 7-8: Begin light strength training with your doctor’s approval
Pay attention to your body and stop if it hurts. Regular exercise helps you recover and lowers the chance of future stomach problems. Always check with your surgical oncology team before starting any new exercise plan after colon resection surgery.
Warning Signs and When to Contact Healthcare Providers
After bowel or colorectal surgery, watch for warning signs. Severe pain, high fever, or a lot of bleeding at the site need quick medical help. These could mean serious problems that need fast treatment.
Also, keep an eye out for changes in bowel habits, constant nausea, or vomiting. These signs might not be as urgent but should be told to your healthcare team. They could mean you need help with your recovery.
If you have sudden chest pain or trouble breathing, call 911 or go to the emergency room. For other concerns or questions about your recovery, reach out to your surgeon’s office. They can tell you if you need to come in or if they can help over the phone.
Being careful and talking to your healthcare providers is key to a safe recovery after surgery. If you’re not sure about any symptoms, it’s always best to ask.
FAQ
Q: What is colon resection surgery?
A: Colon resection surgery, also known as a colectomy, removes part or all of the colon. It treats conditions like cancer, diverticulitis, or inflammatory bowel disease.
Q: How long does colon resection surgery typically take?
A: The surgery’s length varies. It can last from 1 to 4 hours. Laparoscopic procedures are often shorter than open surgeries.
Q: What are the different types of colon resection surgeries?
A: There are several types. These include total colectomy, partial colectomy, and hemicolectomy. The choice depends on the condition being treated.
Q: How long is the hospital stay after colon resection surgery?
A: Hospital stays range from 3 to 7 days. This allows for close monitoring and initial recovery.
Q: What are the possible risks and complications of colon resection surgery?
A: Risks include infection, bleeding, and bowel obstruction. Your surgeon will discuss these risks and how to minimize them.
Q: How long does it take to fully recover from colon resection surgery?
A: Recovery times vary. Laparoscopic surgery recovery is 4 to 6 weeks. Open surgery recovery is 6 to 8 weeks. Recovery times can differ based on the surgery’s extent.
Q: When can I return to work after colon resection surgery?
A: Return to work times vary. Desk jobs may require 2 to 3 weeks. More physically demanding jobs may need 4 to 6 weeks.
Q: What dietary changes should I make after colon resection surgery?
A: You may need a low-fiber diet at first. Gradually add foods back in. Your healthcare provider will give specific dietary guidelines.
Q: Will I need a colostomy bag after colon resection surgery?
A: Not all surgeries require a colostomy bag. In many cases, the colon can be reconnected. Your surgeon will discuss this with you before the surgery.
Q: How soon can I start exercising after colon resection surgery?
A: You can start with light activities like walking soon after surgery. Avoid strenuous exercises for 4 to 6 weeks. Always check with your healthcare provider before starting any exercise.