Blood cancer affects many lives, causing challenges for patients and their families. This guide explores blood cancers like leukemia and lymphoma. It aims to provide key information for those dealing with this diagnosis.
We’ll cover the basics and the latest treatments for blood cancer. Our goal is to give you the knowledge you need. This is for patients, caregivers, and healthcare professionals looking to learn more.
We’ll look at different blood cancers, their symptoms, and new treatments. By sharing medical facts and personal stories, we aim to offer a detailed resource. It will be both scientifically accurate and compassionate.
Understanding Blood Cancer: A Comprehensive Overview
Blood cancer is a complex group of diseases that affect the body’s blood-forming tissues. This overview sheds light on the nature of blood cancer, its impact on the body, and who might be at risk.
What Happens in Blood Cancer
In blood cancer, abnormal cells multiply uncontrollably. This disrupts the normal balance of blood components. These rogue cells interfere with the production of healthy blood cells in the bone marrow, leading to various health issues.
Impact on Blood Cell Production
Blood cancer significantly affects the production of vital blood cells:
- Red blood cells: Carry oxygen throughout the body
- White blood cells: Fight infections
- Platelets: Help with blood clotting
When cancer disrupts this process, it can lead to anemia, increased risk of infections, and bleeding problems.
Who is at Risk
While anyone can develop blood cancer, certain factors increase the risk:
| Risk Factor | Description |
|---|---|
| Age | Risk increases with age, specially after 50 |
| Gender | Some types are more common in males |
| Genetics | Family history can play a role |
| Environmental Exposure | Chemicals like benzene may increase risk |
| Immune System Issues | Weakened immunity can contribute |
Understanding these factors helps in early detection and treatment. For those diagnosed, options like stem cell transplants offer hope in the fight against blood cancer.
Major Types of Blood Cancer
Blood cancer affects how blood cells are made and work. There are three main types, each with its own traits and effects on the body.
Leukemia and Its Variants
Leukemia starts in the bone marrow. It makes too many bad white blood cells. These bad cells take over, making it hard for the body to fight off infections. Leukemia has four main types:
- Acute Lymphoblastic Leukemia (ALL)
- Chronic Lymphocytic Leukemia (CLL)
- Acute Myeloid Leukemia (AML)
- Chronic Myeloid Leukemia (CML)
Lymphoma Classifications
Lymphoma affects the lymphatic system, which fights off germs. It’s split into two main types:
- Hodgkin Lymphoma: Has Reed-Sternberg cells
- Non-Hodgkin Lymphoma: More common, with over 60 subtypes
Multiple Myeloma
Multiple myeloma targets plasma cells in the bone marrow. These cells make bad proteins. This leads to bone pain, kidney issues, and a higher risk of infections. It often starts with a condition called monoclonal gammopathy of undetermined significance (MGUS).
Knowing about these blood cancers helps find them early and treat them better. Each type needs a special plan to manage symptoms and help patients get better.
Early Warning Signs and Symptoms
Spotting blood cancer symptoms early is key for quick diagnosis and treatment. Finding cancer early can greatly help patients. The symptoms can vary by cancer type, but there are common signs to look out for.
Fatigue is often the first sign. It’s not just feeling tired. It’s a deep, lasting exhaustion that doesn’t get better with rest. Unexplained weight loss is also a warning sign, happening fast without diet or exercise changes.
Frequent infections or illnesses that last longer than usual may mean a weak immune system. This is common in many blood cancers. Easy bruising or bleeding, like nosebleeds or bleeding gums, can also point to blood cell issues.
- Persistent fever or night sweats
- Swollen lymph nodes
- Bone or joint pain
- Shortness of breath
- Abdominal discomfort or swelling
If you keep getting these symptoms, see a doctor. These signs don’t always mean you have blood cancer. But, they do need checking out. Early detection can lead to better treatment and outcomes.
The Role of Bone Marrow in Blood Cancer
Bone marrow is key in blood cancer. It’s a spongy tissue in our bones that makes blood cells. Knowing how it works helps us understand blood cancer diagnosis and treatment.
Bone Marrow Function and Structure
Bone marrow is complex. It makes all blood cells. It has stem cells that turn into red, white blood cells, and platelets. These cells carry oxygen, fight infections, and help blood clot.
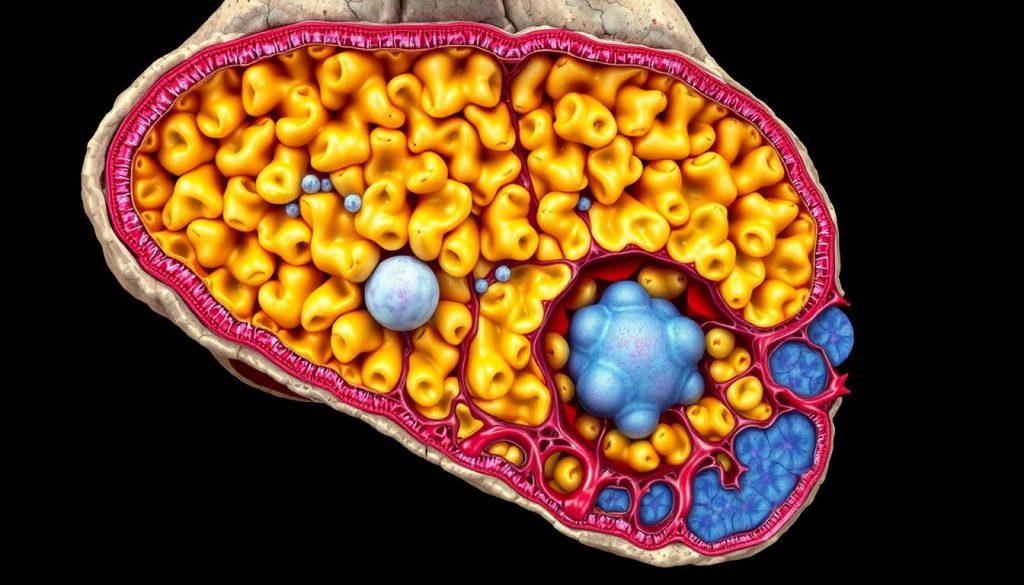
How Cancer Affects Bone Marrow
Blood cancers harm bone marrow. They cause abnormal cells to grow too much. This pushes out healthy cells. This leads to fewer normal blood cells, causing symptoms and problems.
Bone Marrow Biopsy Process
A bone marrow biopsy is a key test for blood cancers. A small bone marrow sample is taken, usually from the hip. Then, it’s checked under a microscope for abnormal cells.
| Biopsy Step | Description |
|---|---|
| Preparation | Patient lies on side, local anesthetic applied |
| Aspiration | Hollow needle inserted, liquid marrow sample drawn |
| Core biopsy | Small piece of bone marrow tissue removed |
| Analysis | Samples examined for abnormal cells |
Understanding bone marrow’s role is vital for those thinking about stem cell transplants. These treatments aim to fix bone marrow, giving hope to blood cancer patients.
Diagnostic Methods and Testing
Getting a blood cancer diagnosis involves several tests. Blood work is usually the first step. It shows if there are any odd cell counts or types.
Imaging tests are also important. X-rays, CT scans, and MRIs help find where the problem is. They show if lymph nodes are big or if bones are damaged. These scans help plan the next steps.
A bone marrow biopsy is a key test. It takes a small sample from the hip bone. This lets doctors check how blood cells are made. They can see if there are cancer cells.
- Complete blood count (CBC)
- Blood smear examination
- Flow cytometry
- Genetic testing
Tests like flow cytometry and genetic analysis give more details. They help find out what kind of blood cancer it is. These tests look at cell markers and genetic changes.
Finding out you have blood cancer takes time. It often needs many tests to be sure. Each test helps doctors understand your cancer better.
Understanding Blood Cancer Staging
Blood cancer staging is key to finding the right treatment. It lets doctors know how far the disease has spread and what the chances of recovery are. This process uses different systems, factors, and methods to assess risk.
Stage Classification Systems
Each blood cancer has its own staging system. For instance, leukemia staging looks at blood cell counts and bone marrow. Lymphomas use the Ann Arbor system, focusing on lymph node regions and organs affected.
Prognostic Factors
Many things affect how well someone will do with blood cancer. These include age, health, genetic changes, and how well they respond to treatment. Doctors use this info to make treatment plans and guess survival chances.
Risk Assessment Methods
Doctors use different tools to figure out a patient’s risk level. These include:
- Genetic testing
- Imaging studies
- Blood tests
- Bone marrow biopsies
These tools help sort patients into low, intermediate, or high-risk groups. This guides treatment choices.
| Risk Level | Characteristics | Treatment Approach |
|---|---|---|
| Low | Favorable genetic profile, good response to initial therapy | Less intensive treatment, close monitoring |
| Intermediate | Mixed risk factors | Standard treatment protocols |
| High | Aggressive disease features, poor initial response | Intensive therapy, clinical trials consideration |
Grasping blood cancer staging is vital for patients and families. It’s the base for making treatment plans that aim to improve life quality and outcomes.
Traditional Treatment Approaches
Blood cancer treatment often uses a mix of old and trusted methods. These methods aim to kill cancer cells while protecting healthy tissues. Let’s look at the main traditional treatments for blood cancers.
Chemotherapy Protocols
Chemotherapy is key in treating blood cancer. It uses strong drugs to kill fast-growing cancer cells. Doctors might use one drug or a mix, based on the cancer type and stage. Chemo can be taken by mouth, injected, or given through an IV.
Side effects of chemotherapy can include hair loss, nausea, and tiredness. But, new drugs help manage these side effects better than before.
Radiation Therapy Options
Radiation therapy uses high-energy beams to kill cancer cells. It’s often used with chemo or before a stem cell transplant. This treatment targets specific areas where cancer cells gather.
Radiation therapy may cause skin changes or tiredness. These effects usually go away after treatment ends.
Surgical Interventions
While less common in blood cancers, surgery can play a role in some cases. It might be used to:
- Remove an affected lymph node
- Insert a port for easier chemo delivery
- Perform a splenectomy in certain situations
| Treatment | Main Use | Common Side Effects |
|---|---|---|
| Chemotherapy | Kill cancer cells throughout the body | Hair loss, nausea, fatigue |
| Radiation Therapy | Target specific cancer sites | Skin changes, tiredness |
| Surgery | Remove affected tissues or insert medical devices | Pain, infection risk |
These traditional approaches are the foundation of blood cancer treatment. They work together to give patients the best chance at recovery.
Advanced Treatment Options
Blood cancer treatment has seen big changes in recent years. New methods bring hope to those who didn’t do well with old treatments. Two big innovations are targeted therapy and immunotherapy.

Targeted therapy targets specific molecules that help cancer grow. It’s different from chemotherapy, which affects all fast-growing cells. This way, it can harm cancer cells less and help patients feel better.
Immunotherapy uses the body’s immune system to fight cancer. It either boosts the body’s defenses or adds synthetic parts to the immune system. This method has been very successful in some blood cancers, leading to long-term remissions.
| Treatment | Mechanism | Potential Benefits |
|---|---|---|
| Targeted Therapy | Attacks specific cancer molecules | Fewer side effects, precise action |
| Immunotherapy | Enhances immune response | Long-lasting remissions, body-wide effect |
These new options mark a move towards personalized medicine in treating blood cancer. Doctors now tailor treatments to each patient and their cancer type. This goal is to get better results and avoid treatments that aren’t needed.
Stem Cell Transplantation Therapy
Stem cell transplantation therapy gives hope to many blood cancer patients. It replaces damaged bone marrow with healthy stem cells. This helps the body make blood cells again.
Autologous Transplants
In autologous stem cell transplants, patients get their own stem cells back. Doctors take these cells before starting chemotherapy. Then, they return them after treatment.
This method lowers the chance of the body rejecting the cells. But, it might not get rid of all cancer cells.
Allogeneic Transplants
Allogeneic transplants use stem cells from a donor. This type of transplant can fight cancer better. The donor cells might attack any cancer cells left behind.
But, it also has a higher risk of complications.
| Transplant Type | Source of Stem Cells | Advantages | Risks |
|---|---|---|---|
| Autologous | Patient’s own cells | Lower rejection risk | Possible cancer cell reintroduction |
| Allogeneic | Donor cells | Potential to fight remaining cancer | Higher risk of graft-versus-host disease |
Recovery and Aftercare
Recovering from a stem cell transplant takes time. Patients stay in the hospital for weeks after the transplant. They need to be watched for infections and other problems.
Aftercare includes regular check-ups, managing medications, and making lifestyle changes. These help support the immune system.
Stem cell transplantation therapy is a key treatment for many blood cancer patients. It can lead to long-term remission or even a cure in some cases. Patients should talk to their healthcare team about the benefits and risks before deciding.
Immunotherapy and Targeted Treatments
Blood cancer treatment has made big strides with immunotherapy and targeted therapies. These new methods use the body’s immune system or target specific cancer cells. They offer hope to many patients.

CAR T-Cell Therapy
CAR T-cell therapy is a new way to fight blood cancers. It changes a patient’s T-cells to attack cancer better. The steps are:
- Collecting the patient’s T-cells
- Genetically modifying them to target cancer cells
- Infusing the modified cells back into the patient
This therapy has shown great promise in treating some leukemia and lymphoma types.
Monoclonal Antibodies
Monoclonal antibodies are proteins made in the lab to target cancer cells. They work by:
- Attaching to cancer cells
- Marking them for destruction by the immune system
- Blocking growth signals in cancer cells
These treatments can fight various blood cancers. They often have fewer side effects than traditional chemotherapy.
Targeted Drug Therapies
Targeted drug therapies aim at specific genetic mutations or proteins in cancer cells. They are different from chemotherapy, which harms all fast-growing cells. Examples include:
- Tyrosine kinase inhibitors for chronic myeloid leukemia
- BTK inhibitors for certain types of lymphoma
- Proteasome inhibitors for multiple myeloma
These treatments can lead to better results and a better life for blood cancer patients.
Clinical Trials and Research Developments
Blood cancer research is moving fast, giving patients new hope. Clinical trials are key to this progress. They test new treatments to find better ways to fight blood cancers.
Patients can join clinical trials to try new therapies. These trials often use targeted drugs that only harm cancer cells. Others aim to boost the immune system to fight cancer better.
Recent breakthroughs in blood cancer research include:
- CAR T-cell therapy: This treatment makes a patient’s immune cells fight cancer.
- Immunotherapy: New drugs help the body’s immune system find and destroy cancer cells.
- Personalized medicine: Treatments made just for a patient’s genetic makeup show promise.
To join a clinical trial, patients should talk to their doctor. They can also search online databases for studies that fit. Being in trials not only gives access to new treatments but also helps future patients.
As research goes on, the outlook for blood cancer patients gets better. Each trial brings us closer to better treatments and possible cures. The future of blood cancer care is brighter than ever, thanks to ongoing research and brave trial participants.
Living with Blood Cancer
Managing blood cancer is more than just treatments. It’s about changing your lifestyle to heal and improve your life. Patients face many challenges, but with the right steps, they can feel normal and well.
Lifestyle Modifications
Small changes in your daily life can make a big difference. Resting and reducing stress are key. Many find meditation or gentle yoga helpful.
It’s vital to stay connected with friends and family while being careful about infections. Creating a supportive home and using assistive devices can make life easier and safer.
Nutrition Guidelines
Eating well is important for managing blood cancer. Foods rich in nutrients help your immune system and energy. Focus on fruits, vegetables, and lean proteins.
Drinking plenty of water is also key. Sometimes, a dietitian can help with specific nutritional needs and side effects from treatment.
Exercise Recommendations
Exercise is great for energy, mood, and life quality for blood cancer patients. Try low-impact activities like walking, swimming, or tai chi. Start slow and listen to your body.
Always talk to your healthcare team before starting any exercise. They can make sure it’s safe for you.
FAQ
Q: What are the main types of blood cancer?
A: Blood cancer includes leukemia, lymphoma, and multiple myeloma. Each affects different blood cells. They have unique subtypes and treatments.
Q: What are common symptoms of blood cancer?
A: Symptoms include fatigue, weight loss, and frequent infections. You might also notice easy bruising, swollen lymph nodes, and bone pain. Night sweats are another sign. Symptoms vary by type and stage.
Q: How is blood cancer diagnosed?
A: Doctors use blood tests, imaging studies, and bone marrow biopsies. These tests help find the type and stage of cancer. They guide treatment choices.
Q: What is a bone marrow biopsy and why is it important?
A: A bone marrow biopsy takes a sample from the hip bone. It’s key for diagnosing and monitoring blood cancers. It checks disease progress and treatment success.
Q: What are the main treatment options for blood cancer?
A: Treatments include chemotherapy, radiation, targeted therapy, immunotherapy, and stem cell transplantation. The right treatment depends on the cancer type, stage, and patient’s health.
Q: What is stem cell transplantation and how does it work?
A: Stem cell transplantation uses healthy stem cells to replace damaged bone marrow. It can be from the patient or a donor. It’s used for aggressive or recurring cancers.
Q: What is CAR T-cell therapy?
A: CAR T-cell therapy genetically modifies T-cells to fight cancer. It’s shown promise in treating some leukemia and lymphoma. It’s a form of immunotherapy.
Q: Are there any clinical trials available for blood cancer patients?
A: Yes, many clinical trials are ongoing for blood cancer. They test new treatments and approaches. Patients should talk to their doctors about eligibility.
Q: How can I maintain my quality of life while living with blood cancer?
A: Quality of life comes from good nutrition, exercise, stress management, and emotional support. Work with your healthcare team to create a personalized plan.
Q: What support resources are available for blood cancer patients and their families?
A: Support includes patient groups, online forums, counseling, and educational materials. Hospitals also offer programs for patients and caregivers.