CAR T cell therapy is a new way to fight cancer. It uses a patient’s own immune system to attack cancer cells. This method has shown great success in treating different types of cancer, giving hope to those who have tried other treatments.
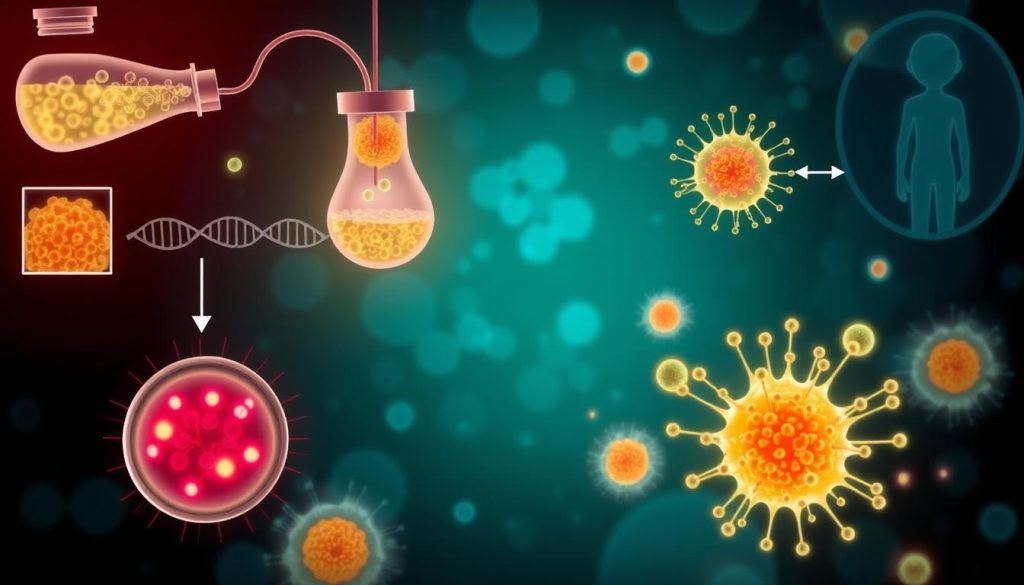
This therapy works by changing a patient’s T cells to find and kill cancer cells. It makes the immune system see cancer as a threat. This could lead to long-term remission for patients with advanced or relapsed cancers.
Researchers are looking into CAR T cell therapy for many cancers. This includes leukemia, lymphoma, multiple myeloma, and even solid tumors. It’s a targeted and personalized treatment, bringing new hope to patients and their families.
What is CAR T Cell Therapy?
CAR T cell therapy is a new way to fight cancer. It uses a patient’s own immune system to attack cancer cells. This method involves adoptive cell transfer, where T cells are taken, changed in a lab, and then sent back to fight cancer.
The therapy’s core is the chimeric antigen receptor (CAR). It’s a man-made part that lets T cells find and kill cancer cells. This makes T cells into gene-modified cells that can target cancer with great accuracy.
- T cells are collected from the patient’s blood through a procedure called leukapheresis.
- The collected T cells are sent to a laboratory, where they are genetically engineered to express the CAR on their surface.
- The gene-modified T cells are multiplied in the laboratory to create millions of cancer-fighting cells.
- The patient undergoes lymphodepleting chemotherapy to prepare their body for the infusion of CAR T cells.
- The CAR T cells are infused back into the patient’s bloodstream, where they can locate and destroy cancer cells.
What makes CAR T cell therapy special is its ability to create a “living drug.” This drug stays in the body and fights cancer for a long time. The T cells can keep working for months or even years, giving some patients long-term protection.
“CAR T cell therapy represents a paradigm shift in cancer treatment, giving hope to patients who have tried everything else.” – Dr. Sarah Johnson, oncologist
While CAR T cell therapy works well for some blood cancers, like leukemia and lymphoma, scientists are exploring its use for other cancers too. As research in adoptive cell transfer and gene-modified cells grows, CAR T cell therapy looks very promising for fighting cancer in the future.
How CAR T Cell Therapy Works
CAR T cell therapy is a complex process. It starts with taking T cells from the patient’s blood. Then, these cells are genetically modified and expanded in a lab. After that, they are given back to the patient.
Harvesting T Cells from the Patient
The first step is T cell extraction, also known as leukapheresis. Blood is drawn and T cells are separated and collected. The rest of the blood is returned to the patient.
Genetically Modifying T Cells
After harvesting, T cells go to a lab for genetic modification. A viral vector is used to add a gene for a chimeric antigen receptor (CAR). This CAR helps T cells target cancer cells better. For more on CAR T cell therapy, check out the American Cancer Society’s page.
Infusing Modified T Cells Back into the Patient
After modification, CAR T cells are expanded to increase their numbers. This ensures enough cells for treatment. Then, they are infused back into the patient’s bloodstream. There, they can find and destroy cancer cells.
| Step | Description |
|---|---|
| 1. T Cell Extraction | T cells are collected from the patient’s blood through leukapheresis. |
| 2. Genetic Modification | T cells are genetically modified using a viral vector to express a CAR specific to the patient’s cancer. |
| 3. Ex Vivo Expansion | Modified CAR T cells are expanded in the laboratory to increase their numbers. |
| 4. Infusion | The expanded CAR T cells are infused back into the patient’s bloodstream to target and destroy cancer cells. |
“CAR T cell therapy represents a significant advancement in personalized cancer treatment, giving hope to patients with hard-to-treat cancers.”
By using the patient’s immune system, CAR T cell therapy can lead to long-lasting remissions. It offers better outcomes for some cancer patients.
Types of Cancer Treated with CAR T Cell Therapy
CAR T cell therapy has shown great success in treating many cancers, mainly hematologic malignancies. This new treatment gives hope to patients with B cell cancers who have tried other treatments without success.
Leukemia and Lymphoma
CAR T cell therapy has been most studied and used for leukemia and lymphoma. It’s been tested on acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL). Studies have shown high response rates and long-term remissions in patients with hard-to-treat diseases.
Multiple Myeloma
Recently, CAR T cell therapy has shown promise in treating multiple myeloma. Early trials have shown good results, with some patients getting deep and lasting responses.
| Cancer Type | CAR T Cell Therapy Indication | Response Rates |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | Relapsed or refractory B-cell ALL | Up to 90% complete remission |
| Diffuse Large B-Cell Lymphoma (DLBCL) | Relapsed or refractory DLBCL | 40-50% complete response |
| Multiple Myeloma | Relapsed or refractory multiple myeloma | Ongoing clinical trials |
Solid Tumors
While CAR T cell therapy has mainly focused on blood cancers, researchers are exploring it for solid tumors. Solid tumors are harder to treat because of the tumor environment and different antigens. But, trials are looking into CAR T cell therapies for various solid tumors, like:
- Glioblastoma
- Neuroblastoma
- Breast cancer
- Prostate cancer
- Ovarian cancer
The success in blood cancers has opened doors for solid tumors. We’re hopeful that more research will make CAR T cell therapy a viable option for more cancers.
As CAR T cell therapy evolves, it brings new hope for patients with few treatment options. Ongoing trials and research in this field are promising for the future of cancer treatment.
Advantages of CAR T Cell Therapy
CAR T cell therapy is a big step forward in cancer treatment. It’s better than old treatments like chemotherapy and radiation. This targeted therapy uses your own immune system to fight cancer cells. It does this without harming healthy tissues too much.

One great thing about CAR T cell therapy is it can lead to durable responses. In studies, many patients saw their cancer go away for a long time. Some have even stayed cancer-free for years. This gives hope to those who’ve tried everything else.
Another plus is it’s a personalized treatment. Each therapy is made just for you, using your own T cells. These T cells are changed to find and kill your cancer. This custom approach might make treatments work better and cause fewer side effects.
“CAR T cell therapy represents a new frontier in cancer treatment, giving hope to those who’ve lost all other options.” – Dr. James Wilson, oncologist
Even though CAR T cell therapy has risks, its benefits are clear. It’s a hopeful option for many fighting advanced cancers. As scientists keep working on it, it could help even more people in the future.
Potential Side Effects and Risks
CAR T cell therapy is a promising treatment for some cancers. But, it’s key for patients to know the possible side effects and risks. The most common issues include cytokine release syndrome (CRS), neurological problems, and B cell aplasia. These happen because the therapy strongly activates the immune system.
Cytokine Release Syndrome (CRS)
CRS is a common side effect, affecting up to 90% of patients. It’s caused by a quick release of cytokines, which are immune system activators. Symptoms can be mild, like fever and flu, or severe, like low blood pressure and organ problems. CRS is usually managed with supportive care and drugs like tocilizumab and corticosteroids.
Neurological Toxicities
Some patients may face neurological side effects, such as confusion and seizures. These issues are thought to be due to CAR T cells entering the brain and causing inflammation. It’s vital to closely monitor and treat these effects with corticosteroids and other supportive measures.
“The side effects of CAR T cell therapy can be severe, but with careful monitoring and the right treatments, most patients can get through these challenges.” – Dr. Sarah Johnson, oncologist
B Cell Aplasia
Because CAR T cell therapy targets CD19 on B cells, it can deplete both cancerous and healthy B cells. This leads to B cell aplasia, making it hard for patients to fight infections. They need long-term immunoglobulin therapy to keep their immune system strong. Researchers are working on therapies that target cancer cells more precisely, reducing harm to healthy B cells.
While the side effects of CAR T cell therapy are concerning, healthcare providers are ready to handle them. With the right patient selection, monitoring, and treatments, the benefits of this therapy often outweigh the risks for many.
Eligibility for CAR T Cell Therapy
Choosing CAR T cell therapy as a treatment is a big decision. It’s important to pick the right patients for the best results. The decision depends on the cancer type, how far it has spread, and the patient’s health.
Usually, this therapy is for people with blood cancers like leukemia, lymphoma, and multiple myeloma. They should have tried other treatments like chemo, radiation, or stem cell transplants without success. Also, they need enough healthy T cells for the treatment process.

Before starting, a team of doctors, nurses, and other experts will check the patient. They look at:
- The patient’s medical history and past treatments
- Physical exams and how well the patient can handle treatments
- Tests to see how far the cancer has spread
- How well the patient can handle possible side effects
The table below shows what makes someone eligible for CAR T cell therapy:
| Criteria | Description |
|---|---|
| Cancer Type | Leukemia, lymphoma, multiple myeloma, or certain solid tumors |
| Treatment History | Refractory to or relapsed after standard treatments |
| Age | Varies by specific therapy, typically adults |
| Performance Status | Adequate organ function and overall health |
It’s key for patients to talk openly with their doctors about CAR T cell therapy. They should discuss the chances of success and possible risks. This way, doctors can choose the best candidates for this new cancer treatment.
CAR T Cell Therapy Treatment Process
The CAR T cell therapy process has several key steps. It starts with an initial evaluation and ends with post-treatment monitoring. Each step is designed to ensure the therapy is safe and effective for each patient. Let’s explore the main steps in this innovative cancer treatment.
Pre-treatment Evaluation
Before starting CAR T cell therapy, patients get a thorough check-up. This includes blood tests, imaging scans, and a look at their medical history. The healthcare team also talks about the therapy’s risks and benefits with the patient and their family.
Leukapheresis
The first step is leukapheresis, or apheresis. The patient’s blood is drawn, and white blood cells, including T cells, are separated. The rest of the blood is returned to the patient. These T cells will be used to make the CAR T cells.
CAR T Cell Manufacturing
The T cells are then sent to a lab for cell processing and genetic modification. Scientists add the CAR gene to the T cells, making them attack cancer cells. This process takes weeks, and patients may get bridging chemotherapy to manage their cancer.
Lymphodepleting Chemotherapy
Before getting the CAR T cell infusion, patients have lymphodepleting chemotherapy. This treatment lowers the immune cells in the body. It makes room for the CAR T cells to grow and reduces the risk of rejection.
CAR T Cell Infusion
After the CAR T cells are made and the chemotherapy is done, they are infused into the patient. This is like a blood transfusion and takes less than an hour. The CAR T cells then multiply and start killing cancer cells.
“CAR T cell therapy offers a personalized approach to cancer treatment, harnessing the power of the patient’s own immune system to fight the disease.” – Dr. Sarah Johnson, Oncologist
Post-treatment Monitoring
After the infusion, patients are watched for side effects or complications. They might stay in the hospital for weeks to ensure their safety. The healthcare team checks on the patient’s response and long-term progress regularly.
Success Rates and Long-term Outcomes
CAR T cell therapy has shown great success in treating advanced blood cancers. It offers hope to patients who have tried other treatments without success. Studies have shown it can lead to long-lasting remissions and improve survival rates for those with leukemia, lymphoma, and multiple myeloma.
In a key trial for patients with relapsed or refractory large B-cell lymphoma, axicabtagene ciloleucel (Yescarta) showed an 82% overall response rate. Fifty-four percent of patients achieved complete remission. The median overall survival was 25.8 months, and the median progression-free survival was 5.9 months. These results highlight CAR T cell therapy’s ability to provide long-lasting remissions.
Another study on tisagenlecleucel (Kymriah) for pediatric and young adult patients with B-cell acute lymphoblastic leukemia found an 81% overall remission rate. Sixty percent of patients achieved complete remission. The median overall survival was 19.1 months, and the median progression-free survival was 11.1 months. This shows CAR T cell therapy’s effectiveness in achieving durable responses.
| CAR T Cell Therapy | Overall Response Rate | Complete Remission Rate | Median Overall Survival | Median Progression-Free Survival |
|---|---|---|---|---|
| Axicabtagene ciloleucel (Yescarta) | 82% | 54% | 25.8 months | 5.9 months |
| Tisagenlecleucel (Kymriah) | 81% | 60% | 19.1 months | 11.1 months |
“CAR T cell therapy has revolutionized the treatment of advanced blood cancers, giving patients a chance at long-term remission and improved overall survival.”
As more patients receive CAR T cell therapy, researchers keep watching the long-term outcomes. While some may see their cancer return, the success rates and long-term outcomes are a big step forward in fighting advanced blood cancers.
Current FDA-approved CAR T Cell Therapies
Several CAR T cell therapies have been approved by the FDA for blood cancers. These treatments use a patient’s immune system to fight cancer. Each therapy targets specific cancer cells and is made just for the patient.
Kymriah (tisagenlecleucel)
Kymriah, made by Novartis, was the first CAR T cell therapy approved in 2017. It helps patients with certain types of leukemia and lymphoma. Kymriah targets B cells and is made to fit each patient’s needs.
Yescarta (axicabtagene ciloleucel)
Yescarta, from Kite Pharma, was approved in 2017 for large B-cell lymphoma. It also targets B cells and is made just for the patient. Clinical trials have shown it can lead to long-lasting remissions.
Tecartus (brexucabtagene autoleucel)
Tecartus, also from Kite Pharma, was approved in 2020 for mantle cell lymphoma. It targets CD19 and is made for each patient. Tecartus has shown promising results in trials, giving hope to MCL patients.
Breyanzi (lisocabtagene maraleucel)
Breyanzi, from Bristol Myers Squibb, was approved in 2021 for large B-cell lymphoma. It targets CD19 and is customized for each patient. Trials have shown it can lead to long-lasting remissions.
These FDA-approved CAR T cell therapies offer hope for blood cancer patients. Scientists are working on new therapies to help more patients.
Cost and Insurance Coverage for CAR T Cell Therapy
CAR T cell therapy is a groundbreaking cancer treatment. But, it comes with significant treatment expenses. The cost can reach hundreds of thousands of dollars, posing a financial challenge for many.
Fortunately, both Medicare and private insurance plans are covering CAR T cell therapy. Medicare, the federal health insurance program, covers FDA-approved CAR T cell therapies when medically necessary. This is for those 65 and older or with certain disabilities.
Many private insurance companies also cover CAR T cell therapy. But, the coverage and out-of-pocket costs vary. This depends on the individual’s insurance plan and the CAR T cell therapy used.
To manage the high treatment expenses, patients can look into financial assistance programs. These are offered by pharmaceutical companies, non-profit organizations, and government agencies. They provide grants, copay assistance, or other financial support to help with the costs.
“CAR T cell therapy has given hope to many cancer patients, but the high cost remains a significant barrier. It’s vital that we work towards making this life-saving treatment more accessible and affordable for all who need it.”
As CAR T cell therapy advances, it’s key for healthcare stakeholders to work together. This includes Medicare, private insurance companies, and policymakers. They need to find solutions to ensure more people can access this innovative cancer treatment while managing the treatment expenses.
Ongoing Clinical Trials and Research
The field of CAR T cell therapy is growing fast. Many clinical trials and research projects are underway. They aim to make the therapy better, safer, and more accessible. Scientists are working on new CAR T cells that target cancer better, last longer, and cause fewer side effects.
These improvements could help treat more types of cancer, even solid tumors. This is exciting news for cancer patients.
One area getting a lot of attention is allogeneic CAR T cells. These are made from healthy donor cells, not the patient’s own. This could make CAR T cell therapy faster and cheaper, reaching more people.
Researchers are also looking into combining CAR T cells with other treatments. This could include checkpoint inhibitors, targeted therapies, and radiation. These combinations might make CAR T cell therapy even more effective and help fight resistant cancers.
| Clinical Trial | Target | Phase |
|---|---|---|
| ALPHA-2 | BCMA | Phase 1 |
| UNIVERSAL | CD19 | Phase 1/2 |
| SURPASS | CD19 + CD20 | Phase 1 |
The table shows some ongoing clinical trials. They’re exploring new CAR T cells and combinations. As research continues, we’ll see even more breakthroughs in CAR T cell therapy. This brings hope to those fighting advanced cancers.
Comparison with Other Cancer Immunotherapies
CAR T cell therapy has been a game-changer for some blood cancers. But, other treatments have also shown great promise. Checkpoint inhibitors like Opdivo and Keytruda block proteins that stop immune cells from fighting cancer. They’ve helped treat melanoma, lung cancer, and more.
Cancer vaccines are another exciting area. They help the immune system find and fight cancer cells. Many vaccines are being tested for breast, prostate, and brain cancers.

CAR T cell therapy is part of adoptive T cell therapy. It takes T cells from a patient, changes them to target cancer, and puts them back. Unlike CAR T cells, TIL therapy uses T cells that already know how to fight cancer.
Each therapy has its own strengths and weaknesses. Checkpoint inhibitors work on many solid tumors but need a strong immune response. Cancer vaccines might offer lasting protection but may not work for advanced disease.
“The future of cancer treatment likely lies in combining different immunotherapies to maximize their effectiveness and overcome resistance mechanisms.”
Scientists are looking into mixing CAR T cell therapy with other treatments. For example, adding checkpoint inhibitors to CAR T cells might help them work better in solid tumors.
Future Prospects and Developments in CAR T Cell Therapy
Researchers are working hard to make CAR T cell therapy even better. They’re using gene editing, like CRISPR, to make CAR T cells more effective. This way, they hope to create cells that can find and kill cancer cells more precisely.
Another big step is making universal CAR T cells. Right now, making CAR T cells for a patient takes a lot of time and money. But universal CAR T cells, made from healthy donors, could be used by many patients. This could make the therapy cheaper and more available.
Synthetic biology is also helping CAR T cell therapy. It lets scientists design new genetic parts for CAR T cells. This could make CAR T cells smarter, so they can fight cancer better.
The future of CAR T cell therapy looks bright. It could change how we treat cancer and help many patients. As scientists keep working, we’ll see even more progress. This brings hope to those fighting cancer.
FAQ
Q: What is CAR T cell therapy?
A: CAR T cell therapy uses your own T cells to fight cancer. First, your T cells are taken out. Then, they are changed to find and kill cancer cells. After that, they are put back into you.
Q: How does CAR T cell therapy work?
A: It uses your immune system to fight cancer. T cells are taken from you, changed to find cancer, and then put back. They then go after and kill cancer cells.
Q: What types of cancer can be treated with CAR T cell therapy?
A: It’s mainly for blood cancers like leukemia and lymphoma. But, it’s also being tested for solid tumors.
Q: What are the advantages of CAR T cell therapy compared to traditional cancer treatments?
A: It’s a targeted therapy that only attacks cancer cells. It’s safer for healthy cells. It also offers a chance for long-lasting remissions and is tailored to each patient.
Q: What are the possible side effects and risks of CAR T cell therapy?
A: Side effects include cytokine release syndrome (CRS) and neurological issues. CRS can cause fever and fatigue, or be severe. Neurological issues might include confusion and seizures. Another risk is B cell aplasia, where T cells attack healthy B cells too.
Q: Who is eligible for CAR T cell therapy?
A: It depends on your cancer type, stage, and health. Those with relapsed or refractory blood cancers are usually candidates. A team will check if you’re a good fit.
Q: What is the success rate of CAR T cell therapy?
A: Success rates vary by cancer type and product. In trials, it’s been 80-90% effective for some cancers. But, not all patients stay in remission, and some may relapse.
Q: How much does CAR T cell therapy cost, and is it covered by insurance?
A: It’s very expensive, over 0,000. Some insurance might cover it, but policies differ. Talk to your team and insurance about costs and help.
Q: What does the future hold for CAR T cell therapy?
A: It’s looking good, with research to make it safer and more effective. Scientists are working on better CAR T cells and cheaper ways to make them. It could change cancer treatment a lot.