Medicine is moving forward with new, effective, and personalized treatments. Cancer immunotherapy is a big hope for those fighting cancer. Targeted immunotherapy, like CAR T cell therapy, is a game-changer. It turns a patient’s immune system into a strong fighter against cancer cells.
This guide helps cancer patients and their families understand CAR T cell therapy. It shows how immunotherapy is changing cancer care. It offers new chances for recovery and better life quality.
Key Takeaways
- Insight into how CAR T cell therapy is at the cutting edge of cancer immunotherapy.
- Understanding the uniqueness of targeted immunotherapy as a prime choice for combating certain types of cancer.
- Recognition of personalized cancer treatment as a means to significantly enhance patient outcomes.
- Enlightenment on the science behind CAR T cell therapy and its role in the patient’s journey towards remission.
- Valuable information on the benefits and potential side effects associated with this innovative treatment.
Understanding CAR T Cell Therapy Immunotherapy
Car t cell therapy immunotherapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. This section will explain what CAR T cell therapy is, its science, and its big impact on cancer treatment.
What is CAR T Cell Therapy?
Chimeric antigen receptor t cell therapy, or CAR T cell therapy, is a new treatment. It makes a patient’s T cells better at finding and killing cancer cells. This is a big step forward in using the body’s immune system to fight cancer.
The Science Behind Chimeric Antigen Receptor T Cells
The heart of this therapy is genetically engineered t cells. Scientists take T cells from a patient’s blood and change them in a lab. They make special receptors called chimeric antigen receptors (CARs) on the T cells.
When these T cells go back into the patient’s body, they can find and destroy cancer cells. This shows how medical technology can work with cells to treat diseases.
Revolutionizing Cancer Treatment Through Immunotherapy
CAR T cell therapy is more than just another treatment. It’s a big change in how we treat cancer. It targets and kills cancer cells, which could mean fewer side effects and better survival rates for patients.
Types of Cancers Treated with CAR T Cell Therapy
The field of cancer cell therapy has made huge leaps forward with CAR T cell therapy. This targeted immunotherapy has changed how we treat blood cancers. It’s now FDA-approved for some types of leukemia and lymphoma, showing great success in fighting these diseases.
Especially, CAR T cell therapy has shown great promise in treating blood cancers like acute lymphoblastic leukemia (ALL), chronic lymphocytic leukemia (CLL), non-Hodgkin’s lymphoma (NHL), and multiple myeloma. For more detailed information on the types of cancers treated, visit CAR T-cell therapy treatment options.
| Cancer Type | Treatment Effectiveness |
|---|---|
| Acute Lymphoblastic Leukemia (ALL) | Highly Effective |
| Chronic Lymphocytic Leukemia (CLL) | Effective with ongoing research |
| Non-Hodgkin’s Lymphoma (NHL) | Very Effective |
| Multiple Myeloma | Effective |
This therapy isn’t just for blood cancers. Researchers are also looking into its use for other types of leukemia and lymphoma. They’re even exploring its use in solid tumors, offering hope for more treatments. The cancer cell therapy field is working hard to make CAR T cells even better for fighting cancer.
As cancer cell therapy and targeted immunotherapy grow, so does the hope for treating more cancers. This means better and more precise treatments for patients and doctors, giving everyone more hope.
The Process of CAR T Cell Therapy
CAR T cell therapy is a new way to fight cancer. It’s a personalized treatment that uses special cells to attack cancer. This method has several important steps to make sure it works best for each patient.
Initial Consultation and Eligibility
The first step is a detailed meeting with doctors. They look at the patient’s health history to see if CAR T cell therapy is right. This makes sure the treatment fits the patient’s needs perfectly.
Collection of T Cells: Apheresis Explained
Next, doctors take T cells from the patient’s blood. This is done through apheresis. It’s a key part of the treatment that helps the T cells focus on cancer cells.
Engineering T Cells to Fight Cancer
Then, the T cells are changed in a lab. They get special tools called CARs that help them find and kill cancer cells. This makes CAR T cell therapy a strong tool in fighting cancer.
| Stage | Description | Purpose |
|---|---|---|
| Initial Consultation | Assessment of patient’s eligibility for CAR T therapy based on medical criteria and cancer type. | To personalize the cancer treatment ensuring safety and effectiveness. |
| Apheresis | Collection of T cells from the patient’s blood. | Enable collection of autologous cells for genetic engineering. |
| Cell Engineering | Modification of T cells to express CARs for targeting cancer cells. | Equip T cells to effectively target and destroy cancer cells. |
Patient Journey: From Diagnosis to CAR T Cell Infusion
The path to car t cell therapy immunotherapy is deeply personal and complex. It’s tailored to each patient’s unique medical needs. This approach not only targets cancer cells more accurately but also shows a strong partnership between the patient and their healthcare team.
When a patient gets a diagnosis, they find out if car t cell therapy immunotherapy is right for them. They go through tests to check the cancer type and stage. They also see if their health can handle the therapy’s challenges.
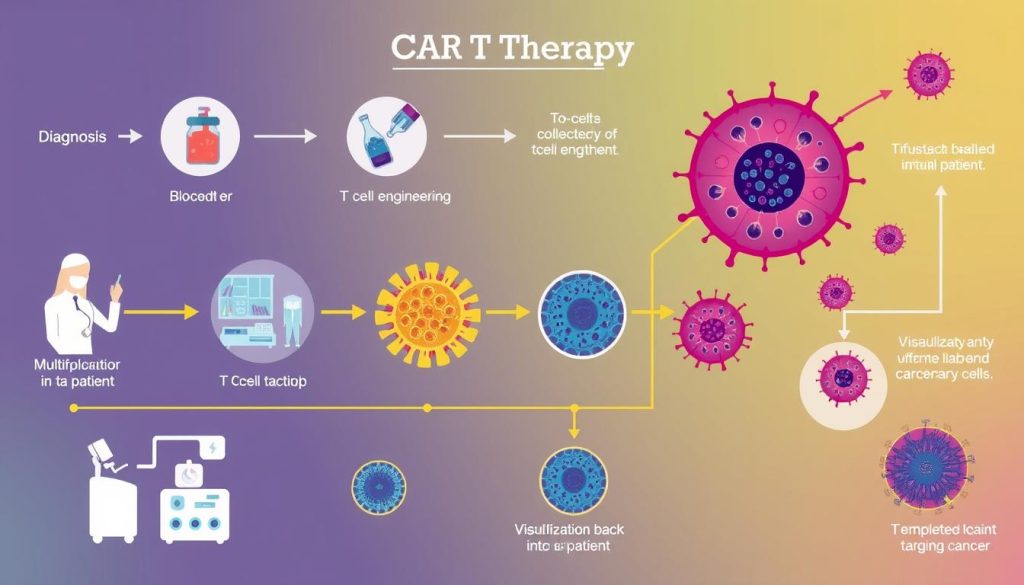
If they’re a good match, the patient starts a series of steps before getting the CAR T cells. First, they collect their T cells. Then, these cells are changed in a lab to better fight cancer.
The preparation is as important as the treatment. It often includes chemotherapy to clear space in the immune system. After that, the modified T cells are given back to the patient. This is a key moment in personalized cancer treatment.
After the infusion, the patient’s progress is watched closely. They have regular check-ups to see how well the therapy is working. This is also when any side effects are managed.
Every step of the treatment is talked about with the patient. They learn about possible side effects, what to expect, and how long it will take. This open talk helps the patient feel involved in their care.
The role of the caregiver is also key during treatment. Their support is vital in dealing with the practical and emotional sides of car t cell therapy immunotherapy.
The Role of Autologous Cell Therapy in Cancer Treatment
Autologous cell therapy is a key part of cancer immunotherapy. It uses a patient’s own cells for treatment. This makes the treatment more effective and reduces the chance of the immune system rejecting it.
This method of personalized medicine is tailored to each patient’s cancer. It targets the cancer precisely and fits the patient’s unique biology.
Personalized Medicine: Tailoring Treatment to the Patient
Personalized medicine is crucial in autologous cell therapy. It involves detailed genetic and molecular profiling. This helps doctors understand how cancer cells grow and avoid the immune system.
They can then modify the patient’s immune cells to attack and destroy cancer cells.
Benefits of Using Patient’s Own Cells for Therapy
Using autologous cell therapy has many benefits. It reduces the risk of immune rejection because the treatment comes from the patient. It also often has fewer side effects than traditional treatments like chemotherapy.
This approach can lead to better outcomes for patients. It shows how cancer immunotherapy and personalized medicine can work together. It has the potential to treat and even cure some cancers by boosting the body’s natural defenses.
The Success Rates and Outcomes of CAR T Cell Therapy
The field of cancer cell therapy has seen a big leap forward. This is thanks to cancer immunotherapy like CAR T cell therapy. Clinical trials show it’s not just effective but can change lives, especially for blood cancer patients.
Measuring a cancer treatment’s success is key. CAR T cell therapy stands out by targeting cancer cells directly. It has shown high remission rates in diseases like acute lymphoblastic leukemia (ALL) and advanced lymphomas.
| Cancer Type | 5-Year Survival Rate Post-Treatment | Remission Duration |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | 40-50% | Long-term (over 5 years) |
| Diffuse Large B-Cell Lymphoma (DLBCL) | 30-40% | Mid-term (1-5 years) |
| Follicular Lymphoma | 35% | Mid-term (1-5 years) |
Even with these good results, scientists keep working to make it even better. They’re improving CAR technology and how it’s used. This could lead to even better results for patients soon.
The cancer immunotherapy community is dedicated to making CAR T cell therapy better. They want to not just extend lives but also improve the quality of life for patients during and after treatment.
Potential Side Effects and How to Manage Them
CAR T cell therapy is a big step forward in fighting cancer. But, it can have side effects that patients should know about. It’s key to understand these effects and how to handle them while getting treatment.
Recognizing CRS: Cytokine Release Syndrome
Cytokine Release Syndrome (CRS) is a common side effect of CAR T cell therapy. It happens when T cells release too many cytokines, causing fever, nausea, and fatigue. In severe cases, it can be life-threatening. It’s important to catch it early and act fast.
Neurological Side Effects and Supportive Care
Neurological problems like confusion and trouble speaking can also happen. Supportive care, like medicine and therapy, helps manage these symptoms. It’s crucial to watch for any changes in the brain and report them right away.
Doctors are always working to make CAR T cell therapy safer and more effective. Patients and their families should talk openly with their doctors. This way, they can deal with side effects quickly and well.
Comparing CAR T Cell Therapy to Conventional Cancer Treatments
Chimeric antigen receptor t cell therapy is a new way to fight cancer. It’s different from old treatments like chemotherapy and radiation. This new method targets cancer cells more precisely, which might mean fewer side effects.
For years, chemotherapy and radiation have been key in fighting cancer. But they can harm healthy cells too, causing big side effects. Targeted immunotherapy, like CAR T cell therapy, attacks cancer cells directly. This helps keep healthy cells safe.

The efficacy of CAR T cell therapy in treating blood cancers is impressive. It uses special T cells to fight cancer better. This has helped many patients who had few options before. Learn more about this therapy at chimeric antigen receptor strategies in cancer.
Even with its success, CAR T cell therapy is still being improved. It works well for blood cancers but needs more work for solid tumors. Solid tumors are harder to treat because of their complex nature.
“The precision of targeted immunotherapy in distinguishing between cancerous and non-cancerous cells introduces a new era in oncology, potentially increasing patients’ quality of life significantly during and after treatment.”
| Treatment Type | Target Specificity | Average Duration of Treatment | Common Side Effects |
|---|---|---|---|
| Chemotherapy | Non-specific | Several months | Hair loss, nausea, fatigue |
| Radiation Therapy | Area-specific | Several weeks to months | Skin irritation, fatigue |
| CAR T Cell Therapy | Highly specific | Varies; typically weeks | Cytokine release syndrome, neurotoxicity |
In conclusion, while old treatments are still important, cancer immunotherapy and chimeric antigen receptor t cell therapy are exciting new options. They could change how we fight cancer in the future.
The Financial Aspect: Insurance and Costs of CAR T Cell Therapy
Understanding the costs of car t cell therapy immunotherapy is key for those thinking about it. This personalized cancer treatment is groundbreaking but comes with a big price tag. We’ll look at the financial side of CAR T Cell Therapy, including insurance and help programs.
Insurance for car t cell therapy immunotherapy changes a lot. It depends on your insurance and the doctor. Most plans see it as a special treatment. But, it’s important to talk to your insurance about what they cover and what you might have to pay.
Because CAR T Cell Therapy is so expensive, many places and groups offer help. They can cover the treatment and other costs like travel. This is because not many places offer this treatment.
| Cost Element | Average Cost | Coverage by Insurance | Assistance Available |
|---|---|---|---|
| Initial Consultation | $350 – $500 | Majority covered | Limited |
| Cell Engineering | $150,000 – $300,000 | Partially covered | Yes |
| Infusion and Hospitalization | $350,000 – $500,000 | Partially to fully covered | Yes |
| Follow-up Care | $25,000 – $75,000 | Partially covered | Possible |
| Travel and Accommodation | $2,000 – $10,000 | Rarely covered | Yes |
It’s crucial for those considering car t cell therapy immunotherapy to talk to doctors, insurance, and support groups. Knowing all about the costs and help available can make things easier. This way, patients can focus on getting better without worrying about money.
A Future of Cancer Treatment: Advancements in CAR T Cell Therapy
The field of cancer immunotherapy is changing fast thanks to CAR T cell therapy. These new steps are making targeted immunotherapy and adoptive cell transfer key in fighting cancer. They offer hope for many types of cancer.
Scientists are working hard to make CAR T cell therapy better. They want to treat more cancers. Finding new ways to fight cancer is very important for the future of treating it.
- Refinement of CAR T cell constructs for increased precision
- Exploration of allogeneic CAR T cells to widen patient eligibility
- Integration of safety switches to improve treatment manageability

As cancer immunotherapy grows, tackling its challenges is key. One big problem is when cancer cells become resistant. New targeted immunotherapy methods are starting to solve this.
| Challenge | Current Strategy | Future Direction |
|---|---|---|
| Limited target antigens | Enhanced target identification processes | Multi-target CARs and tandem CAR T strategies |
| Off-tumor toxicity | Selective receptor targeting | Development of transient CAR T cells |
| Cost and accessibility | Use of autologous cells | Research into off-the-shelf products |
These improvements aim to change how we use adoptive cell transfer. They could lead to better results and help more people. The future of CAR T cell therapy looks bright, offering new hope for cancer patients everywhere.
Support and Resources for Patients Undergoing CAR T Cell Therapy
Going through cancer cell therapy, like CAR T cell therapy, is tough for patients and their families. Many healthcare providers and groups offer help. They provide resources to make the journey easier, following personalized medicine principles.
Patient advocacy groups are key in offering support at every stage of cancer treatment. They share the latest cancer cell therapy info, help with insurance, and more. They also connect patients to counseling for mental health.
- Education on CAR T cell therapy
- Guidance on navigating insurance and financial aid
- Connecting patients to clinical trials and new treatment opportunities
Healthcare facilities also have programs focused on the patient. These programs use personalized medicine to improve treatment results. They might include:
- Workshops on CAR T cell therapy
- One-on-one sessions with oncology social workers
- Access to multi-disciplinary teams for a holistic treatment approach
Community support networks are also very helpful. They offer a sense of belonging and support. Through meetings, forums, and events, they help patients feel less alone.
Health institutions also provide educational materials. These explain the cancer cell therapy process. This helps patients understand and take part in their treatment.
In summary, strong patient support systems are crucial in personalized medicine. They help patients through CAR T cell therapy. They ensure patients don’t face their journey alone.
CAR T Cell Therapy Immunotherapy: Patient Testimonials and Stories
In the world of cancer immunotherapy, patient stories are powerful. They show the personal journeys people take and the big impact of personalized cancer treatment. Here, we look at several patient testimonials that show how CAR T cell therapy can change lives.
“This treatment gave me my life back when I thought all options were exhausted. The tailored approach ensured it worked specifically for my body and cancer type.”
Patient stories often talk about how CAR T cell therapy is made just for them. This is key to personalized cancer treatment. Each story is unique, showing how the therapy fits each person’s fight against cancer.
| Patient Initials | Type of Cancer | Outcome After Treatment |
|---|---|---|
| A.B. | Acute Lymphoblastic Leukemia | Complete remission at 12 months |
| C.D. | Diffuse Large B-Cell Lymphoma | Significant reduction in tumor size |
| E.F. | Follicular Lymphoma | Stable disease with improved quality of life |
The stories of A.B., C.D., and E.F. show how cancer immunotherapy is changing treatment. These stories, from different stages of treatment, show the good and the hard parts of CAR T cell therapy.

These patient testimonials show that CAR T cell therapy is very personal. It’s a treatment that is made just for each person. This makes every patient’s story a sign of the big steps forward in fighting cancer.
The Significance of Targeted Immunotherapy in Oncology
Oncology has seen a big change with targeted immunotherapy. This new way of treating cancer is based on each patient’s genes. It’s a big step forward in cancer immunotherapy.
Targeted immunotherapy attacks cancer cells but not healthy ones. This means fewer side effects and better results.
Moving Beyond One-Size-Fits-All Treatments
For years, oncology used a ‘one-size-fits-all’ approach. This often harmed healthy tissues. But targeted immunotherapy offers a new way.
It focuses on the unique traits of each tumor. This method is more precise and can handle cancer’s genetic variety. It’s a personalized treatment.
Improving Survival Rates with Precision Medicine
Precision medicine has made a big difference in oncology. It uses targeted therapies like CAR T cell therapy. These treatments are much better than old methods.
They use the patient’s genetic markers to create a custom plan. This has led to better results and fewer cancer comebacks.
| Treatment Type | Five-Year Survival Rate Before Precision Medicine | Five-Year Survival Rate After Precision Medicine |
|---|---|---|
| Non-Small Cell Lung Cancer | 15% | 23% |
| Melanoma | 16% | 52% |
| Chronic Lymphocytic Leukemia | 44% | 65% |
Preparing for CAR T Cell Therapy: Tips for Patients and Caregivers
Starting CAR T cell therapy is a big step. It’s important to get ready both emotionally and physically. This treatment is a personalized cancer treatment that needs strong patient support and autologous cell therapy. Here are some tips to help you and your caregivers get ready.
Handling Emotional and Physical Challenges
Recovering from CAR T cell therapy can be tough. It’s key to tackle both the emotional and physical challenges. Being emotionally ready helps a lot with handling side effects and healing.
Seeing a counselor and joining support groups can really help. Sharing experiences with others can be very comforting.
Creating a Support Network for Effective Recovery
Having a strong support network is crucial for recovery. This network should include doctors, family, friends, and community resources. They all work together to give you medical care, emotional support, and help with daily tasks.
| Support Type | Resources | Benefits |
|---|---|---|
| Medical | Oncologists, Nurses, Pharmacists | Direct healthcare and therapy management |
| Emotional | Counselors, Support Groups | Psychological support and coping strategies |
| Practical | Family, Friends, Community Volunteers | Assistance with daily activities and emotional comfort |
Getting ready for CAR T cell therapy means planning well and building a supportive environment. This helps with emotional health and physical recovery. With the right preparation, the journey through CAR T cell therapy can be smoother, leading to better treatment results.
Conclusion
In the world of oncology, CAR T cell therapy immunotherapy is a beacon of hope for cancer patients. This guide has explained CAR T cell therapy’s basics, its process, and its role in cancer immunotherapy. It uses the body’s immune system to fight cancer, showing a step towards personalized medicine.
The path to CAR T cell therapy involves many steps. We’ve looked at the cancers it can treat, the cell collection and reinfusion process, and inspiring patient stories. But, like any new treatment, it also has challenges like side effects and cost. Luckily, there are ways to help with these issues.
As we move into a new era in cancer treatment, CAR T cell therapy’s success is clear. It’s changing cancer care in big ways. With ongoing research and advancements, the future looks bright. CAR T cell therapy is a key part of this hopeful story.
FAQ
Q: What is CAR T Cell Therapy Immunotherapy?
A: CAR T cell therapy is a new way to fight cancer. It uses a patient’s own immune cells, called T cells. These cells are changed to find and attack cancer cells. It’s a personalized treatment that helps the immune system fight cancer better.
Q: How does Chimeric Antigen Receptor T Cell Therapy work?
A: First, T cells from a patient are taken and changed in a lab. They are made to find and mark cancer cells. Then, these changed T cells are given back to the patient to destroy the cancer cells.
Q: What types of cancer can be treated with CAR T Cell Therapy?
A: CAR T cell therapy is mainly for blood cancers like leukemia and lymphoma. But, research is going on to see if it can help with solid tumors too.
Q: What is involved in the initial consultation and eligibility for CAR T Cell Therapy?
A: At the first meeting, a doctor checks if a patient can get CAR T cell therapy. They look at the patient’s health, cancer type, and past treatments. Not everyone can get this therapy, especially if other treatments didn’t work.
Q: What is Apheresis, and how is it related to CAR T Cell Therapy?
A: Apheresis is a way to get T cells from blood. Blood is taken, and the T cells are separated out. Then, the T cells are used to make CAR T cells for treatment.
Q: Why is CAR T Cell Therapy considered a form of personalized medicine?
A: CAR T cell therapy is made just for each patient. It uses their own cells to target their cancer. This makes it a very personal treatment.
Q: What are the success rates and outcomes associated with CAR T Cell Therapy?
A: How well CAR T cell therapy works can vary. For some blood cancers, it can lead to remission. But, results can differ, and patients should talk to their doctors about what to expect.
Q: What are some potential side effects of CAR T Cell Therapy?
A: CAR T cell therapy can cause side effects like Cytokine Release Syndrome (CRS) and neurologic problems. CRS can lead to fever, fatigue, and organ issues. Neurological side effects can range from confusion to seizures.
Q: How do the costs of CAR T Cell Therapy compare to those of conventional cancer treatments?
A: CAR T cell therapy is more expensive than traditional treatments like chemotherapy. But, insurance might help cover some costs. There are also programs to help with the cost.
Q: What advancements are being made in CAR T Cell Therapy?
A: Researchers are working to make CAR T cell therapy better. They want to reduce side effects and use it for more cancers. They’re also trying to make it more affordable and accessible.


















