CAR T-cell therapy is a new hope for cancer patients. It uses the body’s immune system to fight cancer. This approach has shown high remission rates and better survival chances.
As more people try CAR T-cell therapy, knowing its success rates is key. We’ll look at the latest studies and real-world data. This will help us understand how well it works for blood cancer patients.
In this article, we’ll explore CAR T-cell therapy in depth. We’ll cover how it works, its benefits, and its success rates. We’ll also talk about what affects treatment results, side effects, and the future of this therapy.
Introduction to CAR T-Cell Therapy
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to target cancer cells. This method is more precise than traditional treatments like chemotherapy and radiation.
How CAR T-Cell Therapy Works
This therapy starts with changing a patient’s T-cells. T-cells are a type of white blood cell. They are made to find and destroy cancer cells.
First, a blood sample is taken from the patient. T-cells are then taken from this sample. They are changed in a lab to find cancer cells.
After, these changed T-cells are given back to the patient. They then find and kill cancer cells.
Advantages of CAR T-Cell Therapy over Traditional Treatments
There are many benefits to CAR T-cell therapy:
- It targets cancer cells only, which means less harm to healthy cells.
- It’s made just for each patient, making it very personal.
- It can lead to long-term remission, even when other treatments fail.
- It’s given just once, unlike chemotherapy and radiation that need many sessions.
As research goes on, CAR T-cell therapy is changing how we treat cancer. It’s giving hope to many patients.
FDA-Approved CAR T-Cell Therapies
The FDA has approved several CAR T-cell therapies. These treatments give hope to patients with blood cancers like lymphoma, leukemia, and multiple myeloma. They use the body’s immune system to fight cancer, making treatment more personal.
Kymriah (tisagenlecleucel)
Kymriah, made by Novartis, was the first CAR T-cell therapy approved in August 2017. It helps patients up to 25 years old with B-cell precursor acute lymphoblastic leukemia (ALL) that doesn’t respond to treatment. In May 2018, it also got approval for adults with relapsed or refractory large B-cell lymphoma.
Yescarta (axicabtagene ciloleucel)
Yescarta, from Kite Pharma, was approved in October 2017. It’s for adults with relapsed or refractory large B-cell lymphoma after two or more treatments. This includes diffuse large B-cell lymphoma (DLBCL), primary mediastinal large B-cell lymphoma, and high-grade B-cell lymphoma.
Tecartus (brexucabtagene autoleucel)
In July 2020, Tecartus from Kite Pharma got accelerated approval. It’s for adults with relapsed or refractory mantle cell lymphoma (MCL). This was a big step, as Tecartus is the first CAR T-cell therapy for MCL.
Breyanzi (lisocabtagene maraleucel)
Breyanzi, from Bristol Myers Squibb, was approved in February 2021. It’s for adults with relapsed or refractory large B-cell lymphoma after two or more treatments. This includes DLBCL not specified, high-grade B-cell lymphoma, and follicular lymphoma grade 3B.
| Therapy | Manufacturer | FDA Approval | Indications |
|---|---|---|---|
| Kymriah | Novartis | August 2017 May 2018 | B-cell precursor ALL (≤25 years old) Large B-cell lymphoma (adult) |
| Yescarta | Kite Pharma | October 2017 | Large B-cell lymphoma (adult) |
| Tecartus | Kite Pharma | July 2020 | Mantle cell lymphoma (adult) |
| Breyanzi | Bristol Myers Squibb | February 2021 | Large B-cell lymphoma (adult) |
These CAR T-cell therapies have shown great success in trials. They offer a chance for a cure for patients with blood cancers. More treatments are expected to be approved, helping patients with different cancers, including multiple myeloma.
car t-cell therapy success rate
CAR T-cell therapy has changed the game for treating some blood cancers. It gives hope to those who’ve tried everything else. Success is measured by response rates, complete remission, partial remission, and progression-free survival.
In trials, CAR T-cell therapy has shown great results for blood cancers. For example, in relapsed or refractory large B-cell lymphoma, up to 82% of patients respond well. And 54% go into complete remission.
“CAR T-cell therapy has given me a second chance at life. After multiple relapses, I thought I had run out of options, but this innovative treatment brought me into complete remission.” – Sarah, CAR T-cell therapy recipient
In acute lymphoblastic leukemia (ALL), CAR T-cell therapy is also very effective. Complete remission rates are between 70% to 90%. This means patients can live longer without their disease getting worse.
| Cancer Type | Overall Response Rate | Complete Remission Rate |
|---|---|---|
| Large B-cell Lymphoma | 82% | 54% |
| Acute Lymphoblastic Leukemia (ALL) | 81% | 70-90% |
| Multiple Myeloma | 85% | 45% |
While the goal is complete remission, partial remission also improves life quality and survival. As research improves, more patients will get long-term remission and better lives.
Factors Influencing CAR T-Cell Therapy Success
The success of CAR T-cell therapy depends on several key factors. These factors influence patient outcomes. Understanding these factors is important for healthcare providers and patients.

One key factor is patient selection. Age and overall health are important in determining if a patient can get the treatment. Younger patients with fewer health problems tend to do better.
Type and Stage of Cancer
The type and stage of cancer also affect treatment success. Blood cancers like acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL) respond well to CAR T-cell therapy. But, treating more advanced cancers is harder because the disease has spread more.
Previous Treatments and Response
A patient’s treatment history is also important. Patients who have tried many treatments may have harder-to-treat disease. But, those who have responded well to previous treatments might do better with CAR T-cell therapy.
“CAR T-cell therapy offers hope to patients who have exhausted other treatment options, but careful patient selection is essential to maximize the chances of success.” – Dr. Sarah Johnson, oncologist
Healthcare providers consider many factors to decide who will benefit from CAR T-cell therapy. These include age, health, cancer type and stage, and treatment history. This personalized approach is a key part of the growing field of immuno-oncology, bringing new hope to patients and their families.
Clinical Trial Results for CAR T-Cell Therapy
CAR T-cell therapy has shown promising results in clinical studies for various blood cancers. These trials have shown high response rates and durable remissions in patients who have exhausted other treatment options. Let’s take a closer look at the efficacy of CAR T-cell therapy as reported in recent clinical trials.
Response Rates and Durability
Clinical studies have consistently shown impressive response rates in patients treated with CAR T-cell therapy. In a key trial for Kymriah (tisagenlecleucel) in pediatric and young adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL), the overall remission rate was 81% within three months of treatment. Remarkably, the majority of these responses were complete remissions, highlighting the therapy’s efficacy.
The durability of responses is another key aspect. In the same Kymriah trial, the relapse-free survival rate at 6 months was 80%, and the overall survival rate at 12 months was 76%. These findings suggest that CAR T-cell therapy can induce lasting remissions in a significant proportion of patients.
Comparison to Standard Treatments
When compared to standard of care treatments, CAR T-cell therapy has shown superior outcomes in certain blood cancers. For example, in a clinical study of Yescarta (axicabtagene ciloleucel) in adult patients with relapsed or refractory large B-cell lymphoma, the objective response rate was 72%, with 51% of patients achieving a complete response. In contrast, historical data for standard salvage chemotherapy show response rates of only 26% in this patient population.
| Treatment | Overall Response Rate | Complete Response Rate |
|---|---|---|
| Yescarta (CAR T-cell therapy) | 72% | 51% |
| Standard Salvage Chemotherapy | 26% | 8% |
These comparative results underscore the promise of CAR T-cell therapy. It offers superior efficacy and improved outcomes for patients who have failed conventional treatments. As clinical studies continue, it is expected that this innovative approach will reshape the standard of care for certain hematologic malignancies.
Remission Rates in CAR T-Cell Therapy
CAR T-cell therapy has shown great success in treating blood cancers. Complete remission is the main goal, where no cancer cells are found. In trials, CAR T-cell therapy has achieved high complete remission rates, giving hope to those who have tried other treatments.
Some patients also experience partial remission, where cancer is greatly reduced but not gone. Those in partial remission often feel better and have a better quality of life, even with some cancer cells left.
Minimal residual disease (MRD) is another key concept. It’s when a few cancer cells stay after treatment, too small to see with usual tests. Being MRD-negative is a good sign for long-term remission and better survival chances.
Even with CAR T-cell therapy’s success, relapse is a worry for some. Relapse happens when cancer comes back after being in remission. Scientists are working hard to find ways to lower relapse risk and make CAR T-cell therapy last longer.
| Cancer Type | Complete Remission Rate | Partial Remission Rate |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | 70-90% | 10-20% |
| Diffuse Large B-Cell Lymphoma (DLBCL) | 40-50% | 30-40% |
| Multiple Myeloma | 30-50% | 40-60% |
The table shows the high remission rates with CAR T-cell therapy for various blood cancers. While rates differ by cancer type and patient, these results show CAR T-cell therapy’s powerful impact.
Long-Term Outcomes for CAR T-Cell Therapy Patients
As CAR T-cell therapy changes cancer treatment, it’s key to know how patients do long-term. The initial results are good, but we need to look at survival and how long patients stay cancer-free over time.
Studies show CAR T-cell therapy can lead to lasting remissions in blood cancers like ALL and DLBCL. A study in the New England Journal of Medicine found a 52% overall survival rate at 15.4 months for DLBCL patients.
Survival Rates and Quality of Life
Survival is important, but so is how well patients feel after treatment. Many say they feel better and can do normal things again. But, some face long-term side effects like CRS or neurological issues, affecting their life quality.
“CAR T-cell therapy gave me a second chance at life. While the treatment was challenging, I am grateful for the additional time I have had with my family and the opportunity to pursue my passions once again.” – Maria, a CAR T-cell therapy survivor
Monitoring and Follow-Up Care
For the best long-term results, patients need regular check-ups and care. They should see their oncologists often to check their health and watch for cancer signs. Survivorship programs also offer support and resources for life after treatment.
As more data comes in, doctors and researchers will keep improving treatment. They aim to make patients’ lives better and longer.
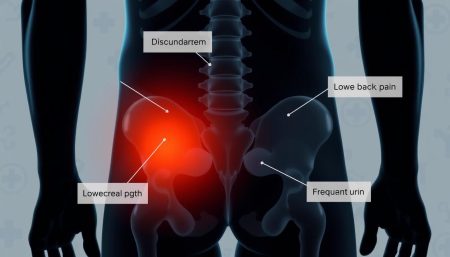
Side Effects and Risks of CAR T-Cell Therapy
CAR T-cell therapy has shown great success in fighting some cancers. But, it comes with possible side effects and risks. It’s important for patients and their caregivers to know about these issues and how to handle them.
Cytokine Release Syndrome (CRS)
One common side effect is cytokine release syndrome (CRS). It happens when the immune system gets too active, releasing inflammatory cytokines quickly. Symptoms can range from mild fever and flu-like symptoms to serious issues like low blood pressure, breathing problems, and organ failure.

Neurological Toxicities
Another risk is neurological toxicity. Patients might feel confused, have seizures, or show other neurological symptoms. These problems need careful watching and quick action from the medical team.
Management and Mitigation Strategies
Healthcare providers use many strategies to manage side effects and keep patients safe. These include:
- Watching patients closely during and after treatment
- Using supportive care like antipyretics, fluids, and oxygen
- Medicines to control the immune system, like corticosteroids
- Tocilizumab, an IL-6 receptor antagonist, for severe CRS
It’s vital for patients getting CAR T-cell therapy to have a skilled medical team. This team should be experienced in handling side effects and providing the right care. With the help of their healthcare providers, patients can face the challenges of treatment and aim for a good outcome.
CAR T-Cell Therapy for Hematologic Malignancies
CAR T-cell therapy is a new way to treat leukemia, lymphoma, and multiple myeloma. It uses the body’s immune system to fight blood cancers. This method is very promising.
First, T cells from the patient are taken and changed to find and kill cancer cells. These T cells are then grown in a lab. After, they are given back to the patient to attack the cancer.
Studies show CAR T-cell therapy works well for blood cancers. It offers hope to those who have tried other treatments. Here are some results from clinical trials:
| Hematologic Malignancy | Response Rate | Complete Remission Rate |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | 81-90% | 60-81% |
| Diffuse Large B-Cell Lymphoma (DLBCL) | 52-82% | 40-54% |
| Multiple Myeloma | 85-95% | 45-50% |
These numbers show CAR T-cell therapy can lead to long-lasting remissions. Dr. James Kochenderfer says it’s a big step forward in cancer treatment.
CAR T-cell therapy represents a major advance in the treatment of hematologic malignancies. The ability to genetically engineer a patient’s own immune cells to recognize and eliminate cancer cells has the potential to revolutionize cancer care.
Even though CAR T-cell therapy is effective against leukemia, lymphoma, and multiple myeloma, more research is needed. It aims to make the treatment even better and to help more people. CAR T-cell therapy is a big hope for those fighting blood cancers.
Emerging Applications of CAR T-Cell Therapy
Scientists are making great strides in research on CAR T-cell therapy. They’re looking into new uses for it, beyond treating some blood cancers. They’re interested in using CAR T-cells to fight solid tumors, which are harder to treat than blood cancers.
They’re working on CAR T-cells that can find and destroy specific cancer cells in solid tumors. This includes cancers like breast, lung, and ovarian. Early clinical trials are starting to see if these new CAR T-cells are safe and work well.
Solid Tumors and Other Cancer Types
Researchers are also exploring CAR T-cell therapy for other cancers. This includes:
- Multiple myeloma
- Chronic lymphocytic leukemia (CLL)
- Hodgkin lymphoma
- Neuroblastoma
Combination Therapies
Another exciting area is combining CAR T-cells with other treatments. This could make treatments more effective and better for patients. Scientists are pairing CAR T-cells with things like checkpoint inhibitors or cancer vaccines.
“The future of CAR T-cell therapy lies in its ability to adapt and expand to treat a wider range of cancers. Through ongoing research and clinical trials, we are pushing the boundaries of what is possible with this revolutionary treatment approach.”
As cancer treatments keep getting better, CAR T-cell therapy is becoming more important. It has the chance to help more people by targeting different cancers and working with other treatments. This could greatly improve the lives of cancer patients all over the world.
Cost and Accessibility of CAR T-Cell Therapy
CAR T-cell therapy is a game-changer for some blood cancers. But, the treatment expenses are a big hurdle for many. The therapy’s unique, personalized approach adds to its high cost.
The price tag for CAR T-cell therapy can reach hundreds of thousands of dollars. This makes it one of the priciest cancer treatments out there. The cost is a challenge for patients and healthcare systems alike, as insurance coverage for it varies a lot.
Many groups and companies offer financial assistance to help with the costs. They provide grants, co-pay help, and other support to those who qualify. This is all about making patient access better.
There’s also a push to make CAR T-cell therapy cheaper. Researchers and industry leaders are working to improve production and lower costs. They aim to make this life-saving treatment more available to those who need it.
“No patient should be denied access to potentially life-saving treatment due to financial constraints. We must work together to ensure that CAR T-cell therapy becomes more affordable and accessible to all who can benefit from it.”
As CAR T-cell therapy shows its worth in treating blood cancers, tackling cost and access issues is key. This will help more patients get this groundbreaking treatment.
Patient Stories and Testimonials
CAR T-cell therapy has changed the lives of many patients with cancer. These brave people have found hope on a journey of recovery. Their stories show the success and promise of this new treatment. Through their experiences, we learn about the emotional impact and better quality of life it can bring.
Sarah, a young mother, was diagnosed with diffuse large B-cell lymphoma. She tried many treatments but then chose CAR T-cell therapy. It worked wonders, and her cancer went into remission quickly. She could regain her strength and enjoy time with her family. Recent studies show that CD19-targeted CAR T cells can lead to long-lasting remissions and even cures for some.

John, a retired teacher, had a relapse of multiple myeloma. He got BCMA-targeted CAR T-cell therapy. It didn’t last as long as CD19-targeted therapies but greatly improved his life. He could enjoy retirement, travel, and time with his grandchildren without the constant hospital visits and symptoms.
“CAR T-cell therapy gave me a second chance at life. It’s not just about the medical outcomes; it’s about the moments I can now cherish with my loved ones.” – John, CAR T-cell therapy patient
These stories show how CAR T-cell therapy can change patients’ lives. It affects not just their health but also their emotional well-being and ability to live fully. As research improves this treatment, more patients will benefit from its life-changing effects.
| Patient | Diagnosis | CAR T-cell Therapy Target | Outcome |
|---|---|---|---|
| Sarah | Diffuse large B-cell lymphoma | CD19 | Prolonged remission |
| John | Multiple myeloma | BCMA | Improved quality of life |
Future Directions in CAR T-Cell Therapy Research
Researchers are working hard to make CAR T-cell therapy better. They want to make it more effective, safe, and easy to get. By looking into new CAR-T technologies and treating more types of cancer, they hope to change cancer treatment for the better.
Gene editing, like CRISPR-Cas9, is a new area of research. It could make CAR T-cells work better and be safer. This means they could target cancer cells more precisely and reduce side effects like cytokine release syndrome (CRS) https://pmc.ncbi.nlm.nih.gov/articles/PMC6746028/.
Improving Efficacy and Safety
Scientists are looking for ways to make CAR T-cells last longer in the body. This could lead to longer-lasting cancer remissions for patients. Some ideas include:
- Adding extra parts to CARs to make them stronger
- Creating CARs that can find and attack more than one cancer antigen
- Using CAR T-cell therapy with other treatments or drugs
Expanding Treatment Indications
So far, CAR T-cell therapy has worked well for some blood cancers. Now, researchers want to use it for solid tumors and other cancers. This is harder because it’s harder to find the right targets and get past the tumor’s defenses.
They’re also looking into using CAR T-cells from donors. This could make the treatment faster and cheaper. It could help more people get the treatment they need.
“The future of CAR T-cell therapy lies in our ability to harness the power of innovative technologies and expand its reach to benefit more patients in need.”
| Research Focus | Potential Impact |
|---|---|
| Gene editing (e.g., CRISPR-Cas9) | Enhanced precision and potency, reduced toxicities |
| Dual-targeting CARs | Improved efficacy and reduced risk of antigen escape |
| Allogeneic (off-the-shelf) CAR T-cells | Increased accessibility and reduced manufacturing time/cost |
The Role of Personalized Medicine in CAR T-Cell Therapy
Precision oncology is changing how we treat cancer, including CAR T-cell therapy. It uses biomarkers and patient stratification to make treatments fit each person better. This approach is making cancer care more effective and promising for the future.
Biomarkers are key in personalized CAR T-cell therapy. They help find out who will benefit most from the treatment. Doctors use biomarkers to sort patients by their unique molecular profiles. This way, they can pick the best CAR T-cell therapy for each person.
Personalized treatment plans are at the heart of CAR T-cell therapy. Doctors consider many factors like age, health, cancer type, and treatment history. This helps create treatments that are more likely to work well. It also reduces the chance of bad side effects, making life better for those getting treatment.
FAQ
Q: What is CAR T-cell therapy?
A: CAR T-cell therapy is a new way to fight cancer. It changes a patient’s T-cells to attack cancer cells. This method has been very successful in treating blood cancers like leukemia and lymphoma.
Q: How does CAR T-cell therapy work?
A: First, T-cells are taken from the patient. Then, they are changed to find and kill cancer cells. After, these special T-cells are given back to the patient to fight the cancer.
Q: What are the advantages of CAR T-cell therapy over traditional treatments?
A: CAR T-cell therapy is better than old treatments like chemo. It only targets cancer cells, not healthy ones. Plus, it keeps working long after treatment ends.
Q: What are the FDA-approved CAR T-cell therapies?
A: The FDA has approved four CAR T-cell therapies. These are Kymriah, Yescarta, Tecartus, and Breyanzi. They help with certain types of leukemia and lymphoma.
Q: What are the success rates of CAR T-cell therapy?
A: CAR T-cell therapy works well for many blood cancers. It can cure up to 90% of patients. But, results can vary based on the cancer type and patient health.
Q: What factors influence the success of CAR T-cell therapy?
A: Success depends on the patient’s health, cancer type, and past treatments. Choosing the right patients can make treatment more effective.
Q: What are the long-term outcomes for CAR T-cell therapy patients?
A: Patients often have long-lasting remissions. But, they need ongoing care and monitoring for side effects.
Q: What are the side effects and risks of CAR T-cell therapy?
A: Side effects include cytokine release syndrome (CRS) and neurological problems. CRS can be mild or severe. Neurological issues can cause confusion and seizures. It’s important to watch for these and treat them quickly.
Q: How much does CAR T-cell therapy cost, and is it covered by insurance?
A: CAR T-cell therapy is very expensive, over 0,000. Insurance coverage varies. Patients may need help to afford it. Efforts are being made to make it more affordable.
Q: What does the future hold for CAR T-cell therapy research?
A: Future research aims to make CAR T-cell therapy better and more available. This includes new technologies and treatments for more cancers. It’s all about improving safety and access.