Cervical cancer is a serious health issue for women around the world. This guide will cover its main points, from early signs to prevention tips. It’s important for women to know about cervical cancer and its link to HPV.
Early detection is key in fighting cervical cancer. Knowing the symptoms and when to see a doctor is vital. We’ll look at screening methods like Pap tests and how they help prevent and catch cancer early.
Preventing cervical cancer is a top priority. There are steps you can take, like getting the HPV vaccine and making healthy choices. By the end of this guide, you’ll know how to protect yourself. Understanding cervical cancer is as important as knowing about oral cancer awareness for your health.
Understanding Cervical Cancer: An Overview
Cervical cancer is a serious health issue for women globally. It happens in the cervix, which is the lower part of the uterus. This part connects to the vagina. We’ll look into what cervical cancer is, how it starts, and its worldwide effect.
What Is Cervical Cancer?
Cervical cancer happens when cells in the cervix grow wrong and keep growing. The main reason is the human papillomavirus (HPV), a common virus spread through sex. Pap tests can find early changes in cervical cells. This helps doctors treat it early.
How Cancer Develops in the Cervix
Cancer in the cervix grows slowly. It begins with changes that can become cancer if not treated. These changes often don’t show symptoms, making screenings key. HPV is the main cause of these changes.
Global Impact and Statistics
Cervical cancer hits women everywhere, with different effects depending on where they live and healthcare access. Here’s a look at its global reach:
| Region | New Cases (2020) | Deaths (2020) |
|---|---|---|
| North America | 13,800 | 4,300 |
| Europe | 58,200 | 25,800 |
| Asia | 319,800 | 168,400 |
| Africa | 119,300 | 81,700 |
These numbers show why we need better access to HPV vaccines, Pap tests, and early diagnosis. This can help fight cervical cancer worldwide.
Early Warning Signs and Symptoms
Knowing the early signs of cervical cancer can save lives. Women should watch for these signs to get medical help early. This can greatly improve treatment chances.
Common Physical Symptoms
In the early stages, cervical cancer often has no symptoms. But as it grows, women might notice:
- Abnormal vaginal bleeding
- Pelvic pain
- Pain during intercourse
- Unusual vaginal discharge
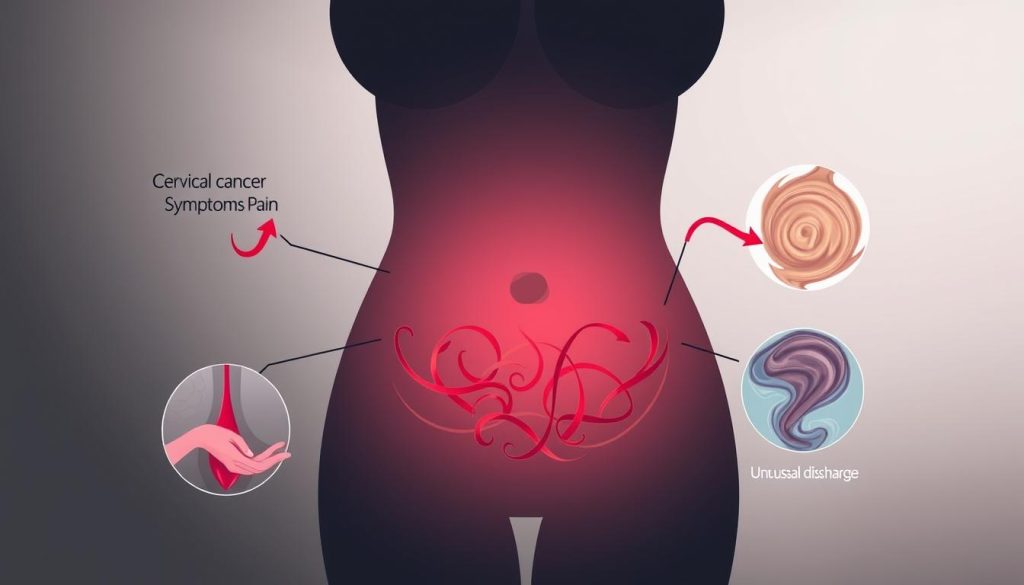
Advanced Stage Indicators
When cervical cancer gets worse, symptoms get more severe:
- Leg pain or swelling
- Difficulty urinating
- Back pain
- Unexplained weight loss
When to See a Doctor
Screening is key for catching cancer early. Women should see a doctor if they notice:
| Symptom | Duration | Action |
|---|---|---|
| Abnormal bleeding | More than 2 weeks | See doctor immediately |
| Pelvic pain | Persistent | Schedule appointment |
| Unusual discharge | Ongoing | Consult gynecologist |
Regular Pap smears can spot cervical changes early. Women aged 21-65 should get screened as advised by their doctor.
The Role of HPV in Cervical Cancer
HPV is a key player in cervical cancer. It infects cells in the cervix, leading to abnormal growth and cancer. Knowing this helps in prevention and early detection.
Most HPV infections go away on their own. But some high-risk strains can stay and cause changes. These changes might turn into cancer if not treated. Regular screenings catch these changes early.
Some HPV types are more likely to cause cancer. Types 16 and 18 are behind about 70% of cervical cancer cases. Knowing your HPV status can help understand your risk.
| HPV Type | Risk Level | Associated Cancers |
|---|---|---|
| 16, 18 | High | Cervical, anal, throat |
| 31, 33, 45, 52, 58 | High | Cervical |
| 6, 11 | Low | Genital warts |
Vaccination is a strong way to prevent HPV infection. The HPV vaccine protects against the most common cancer-causing strains. It works best when given before exposure, usually in adolescence.
Understanding the HPV and cervical cancer link helps us take action. Regular screenings, vaccination, and safe practices lower cervical cancer risk.
Risk Factors and Contributing Causes
It’s important to know about cervical cancer risk factors to prevent it. These include lifestyle choices and genetic predispositions. Knowing your risk can help you protect yourself.
Lifestyle-Related Risk Factors
Some habits can increase your risk of cervical cancer. Smoking weakens your immune system, making it harder to fight HPV infections. Having many sexual partners or starting early can also raise your risk.
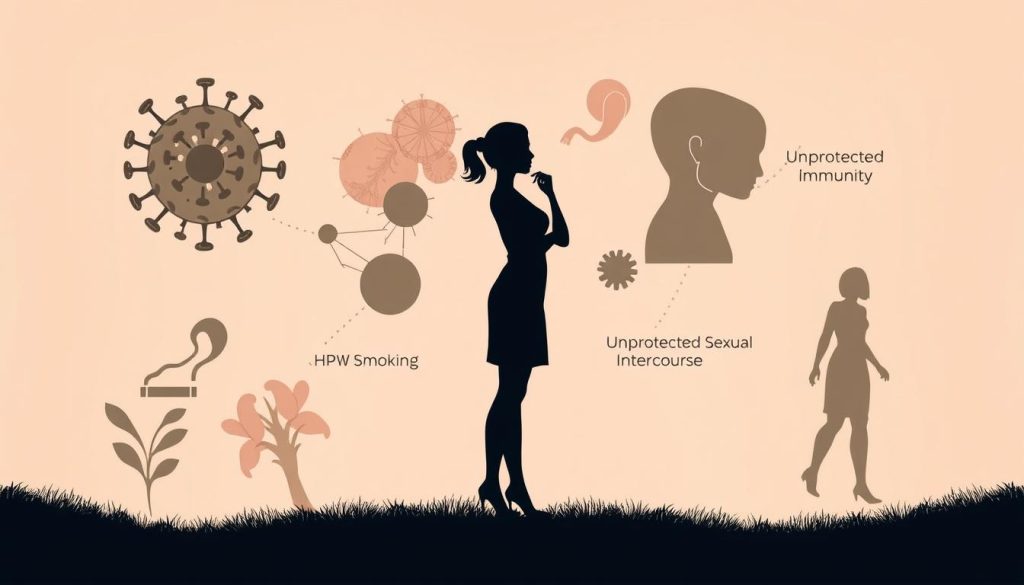
Genetic and Environmental Factors
Your genes can affect your risk of cervical cancer. If your family has a history of it, you might be more at risk. Environmental factors like certain chemicals can also play a part.
Medical History Considerations
Your past health can impact your risk. Long-term birth control use, many children, or a weakened immune system can increase your risk. Regular screenings are vital for early detection and prevention.
- HPV infection
- Smoking
- Weakened immune system
- Long-term birth control use
- Multiple pregnancies
Understanding these risk factors helps you make better health choices. Regular check-ups, HPV vaccination, and lifestyle changes are key to preventing cervical cancer.
Preventive Measures and Screening Tests
It’s important to take steps to prevent cervical cancer. By knowing and using key strategies, you can lower your risk.
HPV Vaccination Guidelines
The HPV vaccine is a key part of preventing cervical cancer. It’s advised for girls and boys starting at 11 or 12. If you missed it, you can get vaccinated up to age 26.
This vaccine protects against HPV types that cause most cervical cancers.
Regular Pap Smear Tests
Pap tests are vital for early detection. Women should start screening at 21 and do it every three years until 65. For those 30 to 65, a Pap test with HPV screening every five years is better.
These tests can find changes that might become cancer before they do.
Lifestyle Prevention Strategies
Your daily choices help prevent cervical cancer. Quit smoking to strengthen your immune system. Practice safe sex to lower HPV risk.
Eat a diet full of fruits and veggies to boost your health. Regular exercise helps keep you healthy and supports your immune system.
Combining vaccination, regular screening, and healthy living is a strong defense against cervical cancer. Talk to your doctor about the best plan for you.
Diagnostic Procedures and Testing Methods
Cervical cancer diagnosis involves several key procedures. The Pap test is a mainstay in finding abnormal cells early. It’s a quick exam where a doctor takes cells from the cervix to look for changes that might lead to cancer.
HPV testing often goes hand in hand with the Pap test. This screening looks for high-risk strains of human papillomavirus linked to cervical cancer. By combining these tests, doctors can spot problems more accurately.

If initial screenings show concerns, doctors might suggest a colposcopy. This procedure uses a special magnifying device to closely examine the cervix. During a colposcopy, the doctor might take small tissue samples for further testing.
| Diagnostic Test | Purpose | Frequency |
|---|---|---|
| Pap Test | Detect abnormal cervical cells | Every 3 years (ages 21-65) |
| HPV Testing | Identify high-risk HPV strains | Every 5 years (ages 30-65) |
| Colposcopy | Examine cervix in detail | As needed based on other test results |
In some cases, imaging tests like CT scans or MRIs help figure out if cancer has spread. These advanced techniques give detailed views of the body’s internal structures.
Knowing about these diagnostic procedures can help ease anxiety and encourage regular screening. Early detection through these methods greatly improves treatment outcomes for cervical cancer.
Staging and Classification of Cervical Cancer
Knowing about cervical cancer staging is key for both patients and doctors. It shows how far the disease has spread and helps decide on treatments. Let’s look at the main ways to classify cervical cancer.
FIGO Staging System
The International Federation of Gynecology and Obstetrics (FIGO) uses a well-known system for cervical cancer staging. It breaks the disease into four stages based on tumor size and spread:
- Stage I: Cancer is only in the cervix
- Stage II: Cancer has spread beyond the cervix but not to the pelvic wall or lower third of vagina
- Stage III: Cancer has spread to the pelvic wall or lower third of vagina
- Stage IV: Cancer has spread to nearby organs or distant parts of the body
TNM Classification
The TNM system gives a detailed look at the tumor (T), lymph node involvement (N), and metastasis (M). This system offers a clearer picture of the cancer’s spread:
| Category | Description |
|---|---|
| T (Tumor) | Size and extent of the main tumor |
| N (Nodes) | Spread to nearby lymph nodes |
| M (Metastasis) | Spread to distant parts of the body |
Understanding Your Diagnosis
Your cervical cancer diagnosis includes staging and other details like tumor grade and type. This full picture helps plan your treatment, which could be surgery, radiation, or chemotherapy. Always talk to your healthcare team about your diagnosis and treatment options to make the best choices for your care.
Treatment Options and Approaches
Cervical cancer treatment has several effective options. The choice depends on the cancer stage, patient health, and personal preferences. Let’s explore the main approaches to fight this disease.
Surgery Options
Surgery is key in cervical cancer treatment. For early-stage cancers, doctors might do a cone biopsy or simple hysterectomy. Advanced cases might need a radical hysterectomy. These procedures aim to remove the tumor and prevent its spread.

Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s often combined with other treatments for better results. External beam radiation and brachytherapy are two common types used for cervical cancer. Patients typically undergo multiple sessions over several weeks.
Chemotherapy Protocols
Chemotherapy involves using drugs to destroy cancer cells throughout the body. It’s frequently used alongside radiation therapy or after surgery. The specific drugs and schedule vary based on the patient’s condition. Side effects can be managed with proper care and support.
| Treatment | Early Stage | Advanced Stage |
|---|---|---|
| Surgery | Cone biopsy, Simple hysterectomy | Radical hysterectomy |
| Radiation | External beam | External beam + Brachytherapy |
| Chemotherapy | Single-agent | Multi-drug regimen |
Each cervical cancer treatment approach has its benefits and risks. Your healthcare team will work with you to create the most effective treatment plan for your situation. Remember, early detection and timely treatment significantly improve outcomes.
Managing Side Effects During Treatment
Cervical cancer treatment can cause many side effects that affect daily life. It’s important to understand and manage these effects to keep quality of life high during treatment.
Patient care during cervical cancer treatment includes dealing with common side effects like fatigue, nausea, and changes in appetite. Doctors suggest eating well, exercising gently, and getting enough rest. Some find help in therapies like acupuncture or meditation.
Each treatment has its own side effects. For example, radiation can cause skin problems and bowel changes. Chemotherapy might lead to hair loss and a higher risk of infections. Managing these side effects needs a plan that fits each patient’s needs.
| Treatment | Common Side Effects | Management Strategies |
|---|---|---|
| Surgery | Pain, limited mobility | Physical therapy, pain medication |
| Radiation | Skin irritation, fatigue | Skin care routines, rest periods |
| Chemotherapy | Nausea, hair loss | Anti-nausea drugs, scalp cooling |
It’s key for patients to talk openly with their healthcare team about side effects. This helps make quick changes to the treatment plan or add more support care. It aims to ensure the best results and comfort during the cervical cancer treatment journey.
Support Systems and Resources
Facing cervical cancer can feel overwhelming, but you’re not alone. There are many support systems and resources to help you and your family. They are here to guide you through this tough time.
Patient Support Groups
Being part of a support group can be very helpful. You’ll meet others who know what you’re going through. They offer emotional support, useful tips, and a sense of community.
Many hospitals and cancer centers have in-person meetings. But, there are also online forums for 24/7 support.

Financial Assistance Programs
Treatment costs can be a big worry. But, there are ways to make it easier. Here are some patient resources:
- Government assistance programs
- Non-profit organizations with grants
- Hospital-based financial counseling services
- Pharmaceutical company patient assistance programs
Counseling Services
Professional counseling is very important during your cancer journey. Therapists who specialize in oncology can help you deal with emotional challenges. They can also help you manage stress and improve your life quality.
Many cancer centers offer counseling services. Or, they can refer you to qualified therapists in your area.
Remember, asking for help is a sign of strength, not weakness. These cervical cancer support services aim to empower you. Don’t hesitate to reach out and use these valuable resources.
Recovery and Follow-up Care
Recovering from cervical cancer treatment is a journey that needs patience and support. Survivors face unique challenges and opportunities for growth. Understanding the recovery process and the importance of follow-up care can greatly improve long-term outcomes.
The road to recovery is different for everyone. Some may recover quickly, while others need more time. Common experiences include fatigue, emotional ups and downs, and adjusting to physical changes. A healthy lifestyle with balanced nutrition and gentle exercise can help in healing.
Follow-up care is key to maintaining health after treatment. Regular check-ups help doctors monitor for cancer recurrence and address side effects. A typical follow-up schedule includes:
- Every 3-6 months for the first two years
- Every 6-12 months for the next three years
- Annual visits after five years
These appointments may involve physical exams, imaging tests, and blood work. Staying committed to this care plan is essential for early detection of any issues.
Cervical cancer survival rates have improved a lot thanks to better treatments and follow-up care. The table below shows five-year survival rates based on stage at diagnosis:
| Stage | 5-Year Survival Rate |
|---|---|
| Localized | 92% |
| Regional | 58% |
| Distant | 17% |
| All Stages Combined | 66% |
Remember, these numbers are averages. Many women live well beyond these estimates. With proper care and a positive outlook, survivors can look forward to fulfilling lives post-treatment.
Latest Research and Medical Advances
The field of cervical cancer research is growing fast. This brings new hope to patients and doctors. Scientists are working hard to find new treatments and ways to prevent the disease.
Emerging Treatments
New therapies are changing how we treat cervical cancer. Immunotherapy uses the body’s immune system to fight cancer. Targeted therapies aim at specific molecules that cause cancer.
Clinical Trials
Clinical trials are key to improving cervical cancer treatment. They test new drugs and ways to treat the disease. Patients in these trials get access to new treatments and help advance cancer care.
Future Perspectives
The future of cervical cancer research is exciting. Scientists are looking into personalized medicine. They’re also exploring new screening methods like AI and blood tests.
As research continues, we’re getting closer to better treatments. Maybe even a cure for cervical cancer.
FAQ
Q: What is cervical cancer?
A: Cervical cancer is a type of cancer that grows in the cervix. This is the lower part of the uterus that meets the vagina. It’s mainly caused by a long-lasting infection with certain types of human papillomavirus (HPV).
Q: What are the early warning signs of cervical cancer?
A: Signs can include abnormal bleeding, pelvic pain, pain during sex, and unusual discharge. But, cervical cancer often has no symptoms in its early stages. That’s why regular screenings are key.
Q: How is cervical cancer diagnosed?
A: Doctors use tests and procedures to find cervical cancer. These include Pap smears, HPV tests, colposcopies, and biopsies. Regular screenings help catch it early.
Q: What is the link between HPV and cervical cancer?
A: HPV is the main cause of cervical cancer. Certain strains of HPV can cause infections that lead to cancer over time.
Q: How can I prevent cervical cancer?
A: To prevent it, get the HPV vaccine and have regular screenings. Practice safe sex, don’t smoke, and live a healthy lifestyle. Vaccination and screenings are the best ways to prevent it.
Q: What are the treatment options for cervical cancer?
A: Treatment depends on the cancer’s stage. It might include surgery, radiation, chemotherapy, or a mix of these. Early-stage cancers might just need surgery, while more advanced ones might need a combination of treatments.
Q: What are the survival rates for cervical cancer?
A: Survival rates depend on when the cancer is found. Early detection leads to a high survival rate. The 5-year survival rate for all stages is about 66%. But, for cancers found early, it’s as high as 92%.
Q: Are there any new treatments or research breakthroughs for cervical cancer?
A: Yes, research is looking into new treatments like immunotherapy and targeted therapies. Clinical trials are also exploring new ways to improve treatment and reduce side effects.
Q: How often should I get screened for cervical cancer?
A: Screening guidelines depend on age and risk factors. Women 21-29 should get a Pap test every 3 years. Women 30-65 can choose a Pap test every 3 years, an HPV test every 5 years, or both every 5 years. Talk to your doctor for the best plan for you.
Q: What support resources are available for cervical cancer patients?
A: There are many resources, like support groups, financial help, and counseling. The American Cancer Society and National Cervical Cancer Coalition offer great information and support for patients and their families.


















