Colorectal cancer is a serious health issue affecting millions globally. This guide covers the main points of this disease. It includes early signs and the latest treatments. Knowing the symptoms and the need for screening can save lives.
Early detection through regular screening is key in fighting colorectal cancer. Spotting symptoms early and getting medical help fast can greatly improve your chances. This detailed guide aims to give you vital information about colorectal cancer, its symptoms, and treatment options.
Understanding Colorectal Cancer: An Overview
Colorectal cancer is a serious health issue affecting millions worldwide. This section will cover the basics of this disease, its development, and its global impact.
What is Colorectal Cancer
Colorectal cancer starts in the colon or rectum. It happens when cells in these areas grow out of control. This cancer often begins as small growths called polyps.
How Cancer Develops in the Colon and Rectum
Cancer development in the colon or rectum is a gradual process. It usually takes years for normal cells to turn into cancer cells. This transformation happens due to changes in DNA.
These changes can be inherited or caused by factors like diet, smoking, or lack of exercise.
Impact on Global Health
Colorectal cancer is a major health issue worldwide. It ranks as the third most common cancer globally. The impact varies across regions due to differences in diet, lifestyle, and screening practices.
| Region | New Cases (2020) | Deaths (2020) |
|---|---|---|
| North America | 151,800 | 53,200 |
| Europe | 519,820 | 244,824 |
| Asia | 958,544 | 478,724 |
Understanding colorectal cancer is key for prevention and early detection. Regular screenings and healthy lifestyle choices can significantly reduce the risk of developing this disease.
Early Warning Signs of Colon and Rectal Cancer
Spotting colorectal cancer symptoms early can save lives. Finding this disease early makes treatment more effective. Knowing the signs helps people get medical help fast.

- Changes in bowel habits lasting more than a few days
- Rectal bleeding or blood in stool
- Persistent abdominal discomfort, such as cramps or pain
- Feeling that your bowel doesn’t empty completely
- Weakness or fatigue
- Unexplained weight loss
These symptoms can also mean other health issues, not just cancer. If you notice any, see your doctor for a check-up.
| Symptom | Description | When to Seek Medical Attention |
|---|---|---|
| Rectal Bleeding | Bright red blood in stool or on toilet paper | Immediately, if it keeps happening |
| Bowel Habit Changes | Diarrhea, constipation, or narrowing of stool | If it goes on for more than a few weeks |
| Abdominal Pain | Cramps, gas pains, or persistent discomfort | If it’s severe or lasts more than a few days |
Early detection through screenings and knowing these symptoms can greatly help. Don’t delay talking to your doctor about any worries.
Common Symptoms That Shouldn’t Be Ignored
Spotting colorectal cancer symptoms early can save lives. Some signs might seem minor, but don’t ignore them. Here are key symptoms you should never overlook.
Changes in Bowel Habits
Bowel changes often signal colorectal problems. You might see:
- Frequent constipation or diarrhea
- Narrower stools than usual
- Feeling like your bowel doesn’t empty completely
These signs can point to issues in your colon or rectum.
Unexplained Weight Loss
Unexpected weight loss is a warning sign for many health issues, including colorectal cancer. If you’re losing weight without trying, it’s time to talk to your doctor about it.
Persistent Abdominal Discomfort
Long-lasting belly pain, cramps, or bloating can mean colorectal problems. While some discomfort is normal, don’t ignore ongoing symptoms.
| Symptom | When to Seek Help |
|---|---|
| Bowel Changes | Lasting more than 2 weeks |
| Weight Loss | 5% or more in 6-12 months |
| Abdominal Pain | Ongoing for several days |
Remember, these symptoms don’t always mean cancer. But they shouldn’t be ignored. Early detection and quick action can greatly improve treatment outcomes.
Risk Factors for Developing Colorectal Cancer
Knowing what increases your risk of colorectal cancer is important. It helps in prevention and early detection. Let’s look at the main risk categories you should know about.
Age and Family History
Your risk of colorectal cancer goes up as you age. Most cases happen after 50. Family history also matters a lot. If your relatives have had colorectal cancer, your risk is higher. That’s why knowing the early signs is key.
Lifestyle Factors
Your daily habits can affect your risk of colorectal cancer. Eating a lot of red and processed meats, not enough fiber, and drinking too much alcohol can up your risk. Smoking and not being active also increase your risk. Staying healthy is a big part of prevention.
Medical Conditions
Some health conditions can make you more likely to get colorectal cancer. These include:
- Inflammatory bowel diseases like Crohn’s or ulcerative colitis
- Type 2 diabetes
- Obesity
- Previous colorectal polyps

| Risk Factor | Impact Level | Prevention Strategy |
|---|---|---|
| Age (50+) | High | Regular screenings |
| Family History | High | Early and frequent screenings |
| Poor Diet | Moderate | Increase fiber, reduce red meat |
| Lack of Exercise | Moderate | Regular physical activity |
| Obesity | Moderate | Maintain healthy weight |
By knowing these risk factors, you can take steps to prevent colorectal cancer. Remember, catching it early through screenings is key for good treatment results.
Diagnostic Methods and Screening Options
Early detection is key in the fight against colorectal cancer. Regular screenings can catch issues before they become serious. Let’s explore the various methods used for colorectal cancer screening and diagnosis.
The gold standard for colorectal cancer screening is the colonoscopy. This procedure allows doctors to examine the entire colon and remove suspicious growths. It’s typically recommended every 10 years for adults over 45.
For those who can’t undergo a colonoscopy, there are other options. Stool-based tests look for hidden blood or altered DNA in feces. These tests are less invasive but need to be done more frequently.
- Fecal Immunochemical Test (FIT): Yearly
- Stool DNA Test: Every 3 years
- Flexible Sigmoidoscopy: Every 5 years
CT colonography, or virtual colonoscopy, uses X-rays to create detailed images of the colon. It’s a good alternative for those who can’t have a traditional colonoscopy.
If these tests reveal anything suspicious, your doctor may recommend a biopsy. This involves taking a small tissue sample for further examination. The results help determine if cancer is present and guide treatment decisions.
Remember, early diagnosis through regular screening can significantly improve outcomes. Talk to your healthcare provider about which colorectal cancer screening method is right for you.
The Importance of Regular Colonoscopy
Regular colonoscopies are key in stopping and finding colorectal cancer early. This test lets doctors check the colon and rectum for any issues or cancer signs.
When to Start Screening
Health experts say to start colorectal cancer screening at 45 for those at average risk. If you have a family history or other risk factors, you might need to start sooner. Always talk to your doctor about what’s best for you.
Preparation Guidelines
Getting ready for a colonoscopy is important for a good test. Here’s what you need to do:
- Follow a clear liquid diet the day before the test
- Take laxatives as directed to clean your colon
- Avoid solid foods and certain medicines as told
- Drink plenty of water during the prep
What to Expect During the Procedure
A colonoscopy is usually done as an outpatient procedure. It takes about 30 to 60 minutes. You’ll be given sedation for comfort. A thin, flexible tube with a camera is inserted into your rectum to look at your colon.

| Aspect | Details |
|---|---|
| Duration | 30-60 minutes |
| Anesthesia | Sedation provided |
| Recovery Time | 1-2 hours after the test |
| Frequency | Every 10 years for average risk |
Remember, regular colonoscopies are vital for catching and preventing colorectal cancer early. Don’t delay in getting your screening done when it’s time.
Understanding Polyps and Their Connection to Cancer
Colorectal polyps are small growths on the inner lining of the colon or rectum. They are key in the development of colorectal cancer. Most start as benign but can turn cancerous over time.
There are different types of colorectal polyps:
- Adenomatous polyps: Most likely to become cancerous
- Hyperplastic polyps: Typically not cancerous
- Inflammatory polyps: Often a result of inflammatory bowel disease
The size and number of polyps impact cancer risk. Larger polyps and more of them raise the cancer risk. Regular screening is vital for early detection and removal of polyps.
| Polyp Size | Cancer Risk | Recommended Action |
|---|---|---|
| Less than 5mm | Very low | Monitor |
| 5-10mm | Low to moderate | Remove and analyze |
| Over 10mm | Higher | Remove and analyze urgently |
Doctors use colonoscopies to find and remove polyps. This is a critical step in preventing colorectal cancer. By taking out polyps early, the risk of cancer drops greatly.
Stages of Colorectal Cancer
Knowing the stages of colorectal cancer is key for planning treatment and understanding the prognosis. Let’s look at the different stages and their survival rates.
Stage I Through IV Explained
Colorectal cancer stages range from I to IV. This shows how far the cancer has spread:
- Stage I: Cancer is in the inner lining of the colon or rectum
- Stage II: Cancer has grown into the wall of the colon or rectum
- Stage III: Cancer has spread to nearby lymph nodes
- Stage IV: Cancer has spread to distant organs like the liver or lungs
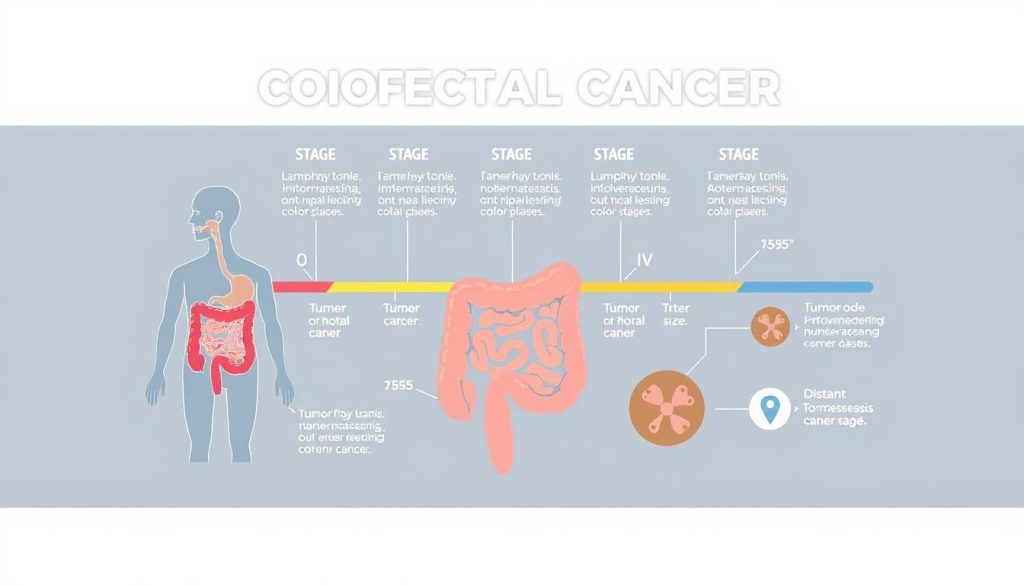
Survival Rates by Stage
Survival rates for colorectal cancer depend on the stage at diagnosis. Here are the five-year survival rates:
| Stage | 5-Year Survival Rate |
|---|---|
| I | 92% |
| II | 63% to 87% |
| III | 53% to 89% |
| IV | 12% |
Keep in mind, these survival rates are averages. Many factors can affect individual outcomes. These include overall health, treatment response, and access to quality care. Early detection through regular screening can improve outcomes. This shows the importance of timely medical check-ups.
Treatment Options and Approaches
Colorectal cancer treatment has many options, each tailored to the patient’s needs. The main treatments are surgery, chemotherapy, and radiation therapy. Let’s dive into each one.
Surgery Options
Surgery is often the first step in treating colorectal cancer. Doctors may remove the tumor and nearby tissue. The type of surgery depends on the cancer’s stage and location.
Chemotherapy Protocols
Chemotherapy uses drugs to kill cancer cells. It’s given in cycles with breaks in between. This method can shrink tumors before surgery or kill any remaining cells after. Some patients get chemotherapy as their main treatment.
Radiation Therapy
Radiation therapy uses high-energy rays to target cancer cells. It’s often used for rectal cancer. It can be given before surgery to shrink tumors or after to kill any leftover cells. Some patients get radiation and chemotherapy together for better results.
| Treatment | Primary Use | Duration |
|---|---|---|
| Surgery | Tumor removal | One-time procedure |
| Chemotherapy | Destroy cancer cells | Several weeks to months |
| Radiation Therapy | Shrink tumors | 5-8 weeks |
Your doctor will create a treatment plan just for you. This plan might include one or more of these treatments. The goal is to give you the best chance at recovery.
Advanced Treatment Technologies
The field of colorectal cancer treatment is changing fast. New technologies are giving patients hope. These new methods aim to make treatments better and less harsh.

Robotic-assisted surgery is a big leap forward. It lets surgeons do complex surgeries with better precision. Patients often feel less pain and recover faster than with old methods.
Immunotherapy is also making waves. It uses the body’s immune system to fight cancer. It’s showing great promise in treating advanced colorectal cancer that was hard to tackle before.
| Advanced Technology | Benefits | Potential Challenges |
|---|---|---|
| Robotic-assisted Surgery | Increased precision, shorter recovery | Higher initial costs, learning curve for surgeons |
| Immunotherapy | Targets specific cancer cells, fewer side effects | Not effective for all patients, possible immune-related side effects |
| Targeted Therapy | Attacks specific cancer-causing molecules | May lose effectiveness over time, regular genetic testing needed |
Targeted therapy is another new way to fight colorectal cancer. These drugs aim at specific molecules that help cancer grow. This makes the treatment more effective and with fewer side effects than traditional chemotherapy.
As research keeps going, these new technologies are leading to better treatments. Patients now have options they couldn’t have dreamed of a few years ago. These options are helping them recover and live better lives.
Recovery and Rehabilitation Process
The journey of colorectal cancer recovery and rehabilitation is very important. It needs careful attention and support. Patients must get guidance on post-surgery care, diet, and physical activity. This helps them regain strength and improve their quality of life.
Post-Surgery Care
After colorectal cancer surgery, proper wound care is key. Patients should keep the incision site clean and dry. They should watch for signs of infection.
Pain management and rest are also important. Regular follow-ups with healthcare providers help ensure proper healing. They also address any complications.
Diet and Nutrition
A balanced diet is vital for colorectal cancer recovery. Patients often need to adjust their eating habits. This supports healing and prevents digestive issues.
Here’s a sample meal plan:
| Meal | Foods to Include | Foods to Avoid |
|---|---|---|
| Breakfast | Oatmeal, banana, low-fat yogurt | High-fiber cereals, citrus fruits |
| Lunch | Grilled chicken, steamed vegetables, rice | Raw vegetables, fried foods |
| Dinner | Baked fish, mashed potatoes, cooked carrots | Red meat, spicy dishes |
Physical Activity Guidelines
Gradual return to physical activity is key for rehabilitation. Patients should start with gentle exercises like short walks. They should progress to more strenuous activities as they regain strength.
Swimming and yoga are excellent low-impact options. They help build endurance and flexibility during colorectal cancer recovery.
Remember, each patient’s recovery journey is unique. It’s important to work closely with healthcare providers. They help create a personalized rehabilitation plan that meets individual needs and goals.
Prevention Strategies and Lifestyle Changes
Controlling your health can greatly lower your risk of colorectal cancer. Making lifestyle changes is key to fighting this disease. Eating a diet full of fruits, vegetables, and whole grains is essential. These foods are packed with nutrients and fiber that boost gut health and fight cancer.
Regular exercise is also vital. Try to do at least 150 minutes of moderate activity or 75 minutes of vigorous activity weekly. Activities like brisk walking, swimming, or cycling are great. Staying at a healthy weight also helps, as obesity is linked to colorectal cancer.
Drinking less alcohol and quitting smoking are musts to lower cancer risk. Both habits can harm cells and cause inflammation, leading to cancer. It’s also key to follow screening guidelines for early detection. Regular screenings can find and remove precancerous polyps, preventing cancer.
By making these lifestyle changes, you’re not just fighting colorectal cancer. You’re improving your overall health and well-being. Remember, even small changes can make a big difference over time. Start now and take control of your colorectal health.
FAQ
Q: What is colorectal cancer?
A: Colorectal cancer starts in the colon or rectum. It begins as a growth called a polyp. Over time, some polyps can turn into cancer.
Q: What are the early warning signs of colorectal cancer?
A: Signs include changes in bowel habits and blood in the stool. You might also feel persistent discomfort or unexplained weight loss. Regular screening is key because many people don’t show symptoms early on.
Q: At what age should I start screening for colorectal cancer?
A: Start screening at 45 if you’re at average risk. If you have a family history or other risk factors, your doctor might suggest starting earlier.
Q: What is a colonoscopy and how often should I have one?
A: A colonoscopy lets doctors check for polyps or cancer. For average risk, it’s every 10 years starting at 45. Your doctor might recommend more often based on your health.
Q: What are the risk factors for developing colorectal cancer?
A: Risk factors include age over 50, family history, and inflammatory bowel disease. Obesity, smoking, and a diet high in red meats also increase risk.
Q: How is colorectal cancer diagnosed?
A: Diagnosis involves screening tests like colonoscopy and biopsies. If cancer is suspected, CT scans help find how far it has spread.
Q: What are the stages of colorectal cancer?
A: Stages range from I to IV. Stage I is local, while Stage IV means it’s spread. The stage affects treatment and outlook.
Q: What treatment options are available for colorectal cancer?
A: Treatments include surgery, chemotherapy, and radiation. The choice depends on the cancer’s stage and your health. Often, a mix of treatments is used.
Q: Can colorectal cancer be prevented?
A: Not all cases can be prevented, but you can lower your risk. Stay healthy, exercise, eat well, and don’t smoke. Regular screenings also help.
Q: What is the survival rate for colorectal cancer?
A: Survival rates vary by stage. Overall, it’s about 65%. But for early-stage cancers, it’s closer to 90%.
Q: How does colorectal cancer affect quality of life during and after treatment?
A: Treatment can affect bowel function and nutrition. It can also impact physical activity and emotional well-being. But, with the right care, many manage well.
Q: Are there any new advancements in colorectal cancer treatment?
A: Yes, new treatments include targeted therapies and immunotherapies. These aim to improve results while reducing side effects.


















