Colorectal cancer symptoms can be hard to spot, making it key to catch them early. Knowing the signs could save your life. This disease often hides until it’s too late, but finding symptoms early can greatly improve your chances.
Look out for changes in your bowel habits or unexplained weight loss. These signs shouldn’t be ignored. Regular screenings are a must, even more so if you’re at higher risk. Don’t wait for symptoms to get worse – catching colorectal cancer early can change everything.
Understanding Colorectal Cancer Symptoms
Colorectal cancer symptoms can be hard to spot. It’s vital to know what to look for to catch it early. This can lead to better health outcomes.
What Defines Early-Stage Symptoms
Early signs of colorectal cancer can seem like other digestive problems. You might notice changes in bowel habits, bleeding, or stomach pain. Not everyone shows the same symptoms.
Why Early Detection Matters
Finding colorectal cancer early can greatly improve your chances of survival. If caught early, the 5-year survival rate is 90%. But, this drops to 14% for more advanced cases. This shows why it’s so important to watch for early signs.
Risk Factors and Symptom Awareness
Knowing your risk factors can help you spot symptoms sooner. Age, family history, and lifestyle choices can increase your risk. Being aware of these can lead to earlier detection and better health.
| Risk Factor | Impact on Symptom Awareness |
|---|---|
| Age (50+) | Increased need for regular screenings |
| Family History | Heightened vigilance for early symptoms |
| Diet High in Red Meat | Monitor for digestive changes |
| Smoking | Pay attention to unexplained weight loss |
By understanding colorectal cancer symptoms, you can take charge of your health. Remember, catching it early through awareness and screenings is the key to successful treatment.
Rectal Bleeding as a Primary Warning Sign
Rectal bleeding is a key sign of colorectal cancer. It can show up as bright red blood in the toilet or darker, tar-like stools. Even if it’s not always cancer, it’s a warning that should not be ignored.
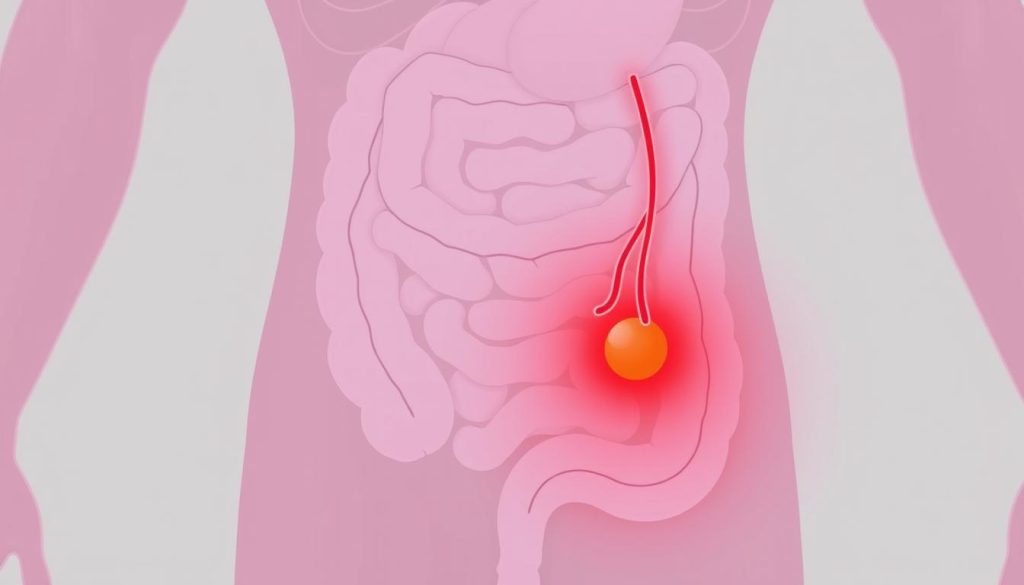
Many people have rectal bleeding at some point. It’s often from harmless things like hemorrhoids or anal fissures. But if it keeps happening or comes with other symptoms, it could mean something serious.
Colorectal cancer symptoms start small. You might see a little blood on toilet paper after wiping. As the disease gets worse, the bleeding gets more obvious. Some people see red streaks in their stool or even pass pure blood.
- Bright red blood usually indicates bleeding from the lower part of the colon or rectum
- Dark red or maroon blood may come from higher up in the digestive tract
- Black, tar-like stools (melena) can suggest bleeding in the upper digestive system
If you notice any rectal bleeding, don’t hesitate to see a doctor. Finding colorectal cancer early can greatly improve treatment chances. Your doctor can run tests to find out why and suggest what to do next.
Changes in Bowel Movement Patterns
A change in bowel habits is a key symptom of colorectal cancer. Your bathroom routine can tell a lot about your digestive health. Let’s look at the changes that might mean you need to see a doctor.
Frequency Changes
Changes in how often you go to the bathroom are important. You might go more or less often. If this lasts more than a few weeks, talk to your doctor.
Consistency Alterations
The texture of your stool can also show problems. Changes in stool consistency, like diarrhea or constipation, could be signs of colorectal cancer. Watch for any unusual changes that don’t go away.
Urgency Issues
Sudden, strong urges to go to the bathroom can be uncomfortable. If you find yourself rushing to the bathroom more, it’s a sign. This could be related to colorectal cancer symptoms.
Not all bowel habit changes mean cancer. But, if you have any of these symptoms for a long time, get medical advice. Early detection can greatly improve treatment outcomes for colorectal cancer.
| Bowel Change | Possible Indication | When to Seek Help |
|---|---|---|
| Frequency Shift | Digestive Issues | After 2-3 weeks |
| Consistency Change | Potential Colorectal Problems | If persistent |
| Increased Urgency | Possible Colon Irritation | When disruptive to daily life |
Persistent Abdominal Discomfort and Pain
Many people feel abdominal pain. If it doesn’t go away, it might be a sign of colorectal cancer. This pain is often different from usual stomach aches.
Those with colorectal cancer might feel a dull ache or cramps in their lower belly. This pain can last for days or weeks. It’s not always very bad, but it doesn’t disappear quickly.

The pain’s location can change. Some feel it on the left, others on the right. Sometimes, the whole lower belly hurts. This pain doesn’t usually get better with common medicines.
Not all abdominal pain means cancer. But if your pain lasts more than a few days, see a doctor. They can find out what’s causing your discomfort.
| Characteristic | Typical Stomach Ache | Potential Colorectal Cancer Pain |
|---|---|---|
| Duration | Hours to a few days | Weeks or longer |
| Location | Often upper abdomen | Lower abdomen, may be on one side |
| Response to OTC meds | Usually improves | Often doesn’t improve |
| Associated symptoms | Nausea, bloating | Changes in bowel habits, weight loss |
Early detection is key in treating colorectal cancer. If you’re worried about ongoing abdominal pain, don’t hesitate to seek medical advice.
Unexplained Weight Loss and Appetite Changes
Unexplained weight loss can be a sign of serious health issues, like colorectal cancer. When the body fights cancer, it can change how much you weigh and how hungry you feel. It’s important to notice these changes early to get help quickly.
Sudden Weight Changes
Fast weight loss without changing your diet or exercise is scary. In colorectal cancer, tumors might use up more calories, causing weight loss. If you lose 10 pounds or more without trying, see a doctor right away.
Loss of Appetite Patterns
Colorectal cancer can make you lose your appetite. You might feel full fast or not want to eat your favorite foods. This loss of appetite often goes with other symptoms like stomach pain or nausea.
Metabolic Changes
Cancer can change how your body uses food and energy. This can make you tired, weak, and lose more weight. Watching how tired you feel, along with your weight, is key.
| Warning Sign | Potential Indication | Action Required |
|---|---|---|
| Unexplained 10+ lb weight loss | Possible colorectal cancer | Consult doctor immediately |
| Sudden loss of appetite | Digestive system changes | Track eating habits, seek medical advice |
| Feeling full quickly | Tumor pressure on organs | Report to healthcare provider |
| Unexplained fatigue with weight loss | Metabolic changes due to cancer | Schedule a thorough health check |
Fatigue and Weakness: Hidden Warning Signs
Feeling tired all the time? It might be more than just a busy lifestyle. Fatigue and weakness can be hidden warning signs of colorectal cancer symptoms. Many people brush off these feelings, but they deserve attention.
Cancer-related anemia often causes persistent tiredness. As the disease progresses, it can drain your energy, leaving you feeling weak and exhausted. This isn’t your typical end-of-day tiredness. It’s a deep, ongoing fatigue that doesn’t improve with rest.

If you’re experiencing unexplained fatigue along with other symptoms, it’s vital to talk to your doctor. They can help determine if your tiredness is related to colorectal cancer or another health issue.
| Normal Tiredness | Possible Cancer-Related Fatigue |
|---|---|
| Improves with rest | Persists despite adequate sleep |
| Linked to daily activities | Unrelated to exertion |
| Temporary | Ongoing for weeks or months |
| Doesn’t interfere with daily life | Impacts ability to function normally |
Remember, fatigue alone doesn’t mean you have cancer. But when combined with other colorectal cancer symptoms, it’s a sign you shouldn’t ignore. Listen to your body and seek medical advice if you’re concerned about persistent fatigue or weakness.
Understanding Anemia in Colorectal Cancer
Anemia is often a hidden sign of colorectal cancer. It happens when there are not enough red blood cells. This can be due to bleeding from tumors in the colon or rectum.
Iron Deficiency Signs
Iron deficiency often leads to anemia in people with colorectal cancer. Look out for:
- Unusual fatigue
- Pale skin
- Shortness of breath
- Dizziness
- Brittle nails
These symptoms can sneak up on you. They might not seem serious at first. But, regular doctor visits can catch iron deficiency early. This could reveal colorectal cancer symptoms.
Blood Count Abnormalities
Blood tests can show signs of colorectal cancer. A complete blood count (CBC) might show:
| Blood Component | Normal Range | Anemic Range |
|---|---|---|
| Hemoglobin | 13.5-17.5 g/dL (men) 12.0-15.5 g/dL (women) | Below 13.5 g/dL (men) Below 12.0 g/dL (women) |
| Hematocrit | 38.8-50% (men) 34.9-44.5% (women) | Below 38.8% (men) Below 34.9% (women) |
Low hemoglobin or hematocrit levels mean you might have anemia. If these levels don’t get better, you might need more tests for colorectal cancer.
Narrowing of Stools: What It Means

A change in your stool’s shape or size can be a red flag for your health. One key sign to watch for is the narrowing of stools. This symptom might point to colorectal cancer symptoms that need attention.
When stools become thinner than usual, it’s often due to an obstruction in the colon or rectum. Tumors can grow and create a blockage. This forces waste to squeeze through a smaller opening. As a result, stools become pencil-thin or ribbon-like.
Keep in mind that narrowing of stools isn’t always caused by cancer. Other conditions like hemorrhoids or anal fissures can lead to similar changes. But if you notice this symptom persisting for more than a few weeks, it’s important to speak with your doctor.
Early detection of colorectal cancer symptoms can make a big difference in treatment outcomes. Don’t ignore changes in your bowel habits, even if they come with other signs like:
- Blood in your stool
- Unexplained weight loss
- Constant fatigue
- Abdominal pain or cramping
Remember, your body sends signals when something’s not right. Paying attention to these signs and seeking medical advice promptly can be life-saving. If you’re concerned about narrowing stools or any other symptoms, reach out to your healthcare provider for proper evaluation and guidance.
Digestive Issues and Persistent Gas
Digestive problems can point to serious health issues, like colorectal cancer. Knowing when bloating and gas pain are a concern is key. This can help you know when to see a doctor.
Bloating Patterns
Bloating is common, but some patterns might mean something serious. If bloating doesn’t get better with diet changes or over-the-counter meds, it’s a warning sign. Watch for bloating with other symptoms like stomach pain or changes in bowel movements.
Gas Pain Characteristics
Gas pain from colorectal cancer is different from usual stomach discomfort. It might be more intense, last longer, or hurt in certain spots. Look out for:
- Pain that doesn’t go away after passing gas or having a bowel movement
- Discomfort that gets worse over time
- Sharp or cramping pain in the lower abdomen
- Gas pain with other digestive problems like constipation or diarrhea
While some digestive issues are normal, persistent ones need attention. If you have ongoing bloating, unusual gas pain, or other digestive symptoms, see your doctor. Catching colorectal cancer early can greatly improve treatment chances.
When to Seek Medical Attention
Knowing when to see a doctor for colorectal cancer symptoms is key. If your bowel habits change or you notice odd signs, it’s time to visit a healthcare provider.
Don’t ignore these possible colorectal cancer symptoms:
- Rectal bleeding or blood in stool
- Unexplained weight loss
- Ongoing abdominal pain or discomfort
- Persistent changes in bowel movements
- Fatigue that doesn’t improve with rest
These signs might not always mean cancer, but they need quick checking. If you’re over 50 or have a family history of colorectal cancer, regular screenings are a must. Don’t wait for symptoms to get worse before getting help.
Early detection is life-saving. If you’re worried about symptoms, make an appointment with your doctor. They can check if more tests are needed and give you peace of mind. Your health is worth the call.
Diagnostic Tests for Symptom Evaluation
When symptoms of colorectal cancer appear, doctors run various tests to find out if it’s cancer. These tests are vital for catching cancer early and planning treatment.
Screening Options
Regular screening is essential to find colorectal cancer early. Here are some common screening methods:
- Colonoscopy: A visual exam of the entire colon using a flexible tube with a camera
- Fecal occult blood test: Checks for hidden blood in stool samples
- Flexible sigmoidoscopy: Examines the lower part of the colon
- Stool DNA test: Looks for altered DNA in stool
Advanced Testing Methods
If initial screenings show a problem, doctors might use more advanced tests:
- CT colonography: Creates detailed images of the colon using X-rays
- Biopsy: Removes tissue samples for lab analysis
- Blood tests: Check for anemia and tumor markers
These tests help doctors understand colorectal cancer symptoms better. Early detection through regular screening can greatly improve treatment results. If you notice any unusual symptoms, talk to your doctor about the right tests.
Age-Related Risk Factors and Symptoms
Age is a big factor in colorectal cancer risk. As we get older, our risk goes up. Knowing how age affects symptoms is key for catching it early.
Colorectal cancer used to be seen as a disease for older people. Those over 50 were thought to be at the highest risk. This led to screening mainly for this age group. But, there’s a worrying change now.
Younger adults are seeing more cases of colorectal cancer. This shows we need to be aware at all ages. It’s important to know that symptoms can show up at any age.
| Age Group | Risk Level | Recommended Screening |
|---|---|---|
| Under 45 | Low to Moderate | If symptoms present or family history |
| 45-75 | Moderate to High | Regular screenings recommended |
| Over 75 | High | Individualized screening plans |
Age is important, but not the only thing. Family history, lifestyle, and health also matter. No matter your age, knowing the symptoms is key. Look out for changes in bowel habits, unexplained weight loss, or rectal bleeding.
Early detection is critical. Stay informed about your risk and talk to your doctor about any worries.
Family History and Symptom Awareness
Understanding your family history is key to knowing your risk for colorectal cancer. Knowing your genetic background helps you watch for symptoms and take steps to prevent it.
Genetic Predisposition
Some families have genetic mutations that raise the risk of colorectal cancer. If your relatives have had this disease, you might have these genes too. It doesn’t mean you’ll definitely get cancer, but your risk goes up.
Inherited Risk Patterns
Certain inherited conditions can greatly increase your risk of colorectal cancer. These include:
- Lynch syndrome
- Familial adenomatous polyposis (FAP)
- MUTYH-associated polyposis
If these conditions are in your family, talk to a healthcare provider about your risk. They might suggest earlier or more frequent screenings to catch symptoms early.
| Family History | Recommended Screening Age | Screening Frequency |
|---|---|---|
| No family history | 45 years | Every 10 years |
| One first-degree relative | 40 years or 10 years before relative’s diagnosis | Every 5 years |
| Lynch syndrome | 20-25 years | Every 1-2 years |
Knowing your family history gives you power over your health. Be alert to colorectal cancer symptoms and follow screening guidelines based on your risk.
Lifestyle Factors Affecting Symptom Development
Your daily choices greatly impact colorectal cancer symptoms. What you eat, how active you are, and other habits matter. Let’s look at how lifestyle affects these symptoms.
Diet is very important. Eating a lot of red meat and processed foods can raise your risk. But, a diet full of fruits, veggies, and whole grains can help protect you.
Being active is also key. Regular exercise can lower your risk of colorectal cancer symptoms. Try to do at least 30 minutes of moderate activity every day.
Smoking and drinking too much alcohol can harm your colon. These habits may cause early signs of colorectal cancer. Quitting smoking and drinking less can help a lot.
| Lifestyle Factor | Impact on Colorectal Cancer Symptoms |
|---|---|
| High-fiber diet | Reduces risk of symptoms |
| Regular exercise | Lowers chance of symptom development |
| Smoking | Increases likelihood of symptoms |
| Excessive alcohol | May contribute to symptom onset |
By choosing healthy lifestyles, you can lower your risk of colorectal cancer symptoms. Remember, early detection through screenings is key. If you notice any unusual changes, talk to your doctor right away.
Prevention Strategies and Regular Screening
Preventing colorectal cancer is key to staying healthy. Regular screenings help catch problems early. The American Cancer Society says adults should start screening at 45.
Screening Guidelines
There are several screening options like colonoscopy and stool tests. Your doctor will choose the best one for you. Early detection can greatly improve treatment results.
Prevention Methods
There are ways to lower your risk of colorectal cancer. Eating more fruits, veggies, and whole grains is helpful. Also, exercising regularly and not smoking are important.
Lifestyle Modifications
Small changes can greatly improve your health. Drinking less alcohol, staying hydrated, and managing stress are good habits. By making these changes, you can lower your risk of colorectal cancer.
FAQ
Q: What are the most common early warning signs of colorectal cancer?
A: Early signs of colorectal cancer include rectal bleeding and changes in bowel habits. You might also feel persistent abdominal discomfort, unexplained weight loss, and fatigue. Remember, these symptoms can also mean other health issues. But if they keep happening or get worse, see a doctor.
Q: How important is early detection in colorectal cancer?
A: Finding colorectal cancer early is key. If caught early, the survival rate can hit 90% within five years. Regular screenings and quick action to symptoms can greatly improve your chances of beating the disease.
Q: What should I do if I notice blood in my stool?
A: Seeing blood in your stool is a big warning sign. You should talk to a doctor right away. It might not always be serious, but it’s always worth checking out. Your doctor will likely suggest more tests to figure out what’s going on.
Q: How do changes in bowel habits relate to colorectal cancer?
A: Changes in your bowel habits, like diarrhea or constipation, could be early signs. If these changes last more than a few weeks, it’s time to talk to your doctor.
Q: Can unexplained weight loss be a sign of colorectal cancer?
A: Yes, losing weight without trying can be a sign of colorectal cancer. If you’re losing weight and feeling tired or noticing changes in your bowel habits, see a doctor.
Q: How does anemia relate to colorectal cancer?
A: Anemia, or low iron, can be a sign of colorectal cancer. Tumors can cause slow blood loss, leading to anemia. Symptoms include feeling very tired, weak, and short of breath.
Q: What does narrowing of stools indicate?
A: Narrowing of your stools might mean there’s a tumor blocking your stool. If your stools are getting thinner, talk to your doctor right away.
Q: At what age should I start getting screened for colorectal cancer?
A: The American Cancer Society says start screening at 45 if you’re at average risk. But if you have a family history or other risk factors, you might need to start earlier. Your doctor will help figure out when you should start.
Q: How does family history affect my risk of colorectal cancer?
A: Family history can raise your risk of colorectal cancer. If a close relative has had it, your risk is higher. Tell your doctor about your family history to get the right screening advice.
Q: Can lifestyle changes help prevent colorectal cancer?
A: Yes, making healthy lifestyle choices can lower your risk. Stay at a healthy weight, exercise, drink less alcohol, don’t smoke, and eat lots of fruits, veggies, and whole grains. Try to limit red and processed meats too.


















