Dealing with women’s health issues means understanding unique conditions. PCOS and menopause are complex and need clear guidance. Women worldwide face PCOS symptoms and menopause without a detailed guide to help manage their symptoms and keep hormonal balance.
PCOS and menopause mark a big change in a woman’s life. It’s important to know how to handle these changes for her well-being. The path through PCOS and menopause varies greatly for each woman. This guide aims to provide insight and support during this life-changing time.
Understanding PCOS and Its Impact on Women’s Health
Polycystic ovary syndrome (PCOS) affects millions of women worldwide. It impacts not just reproductive health but also long-term health due to hormonal imbalance.
What is Polycystic Ovary Syndrome?
PCOS is when a woman’s body makes too many male hormones. This can stop eggs from being released during ovulation. The National Institutes of Health says it’s a top reason for female infertility.
How PCOS Affects Long-term Health
Women with PCOS are at higher risk for serious health issues. These include type 2 diabetes, high blood pressure, and heart disease. They also face mental health problems like anxiety and depression. Managing PCOS is key to women’s health care.
The Connection Between PCOS and Hormonal Imbalance
The Endocrine Society explains how PCOS hormonal imbalance leads to metabolic problems. Insulin issues in PCOS increase the risk of metabolic syndrome. This makes managing women’s health even more complex.
To understand PCOS’s impact on women’s health, let’s look at hormone levels:
| Hormone | Normal Range | Range in Women with PCOS |
|---|---|---|
| Testosterone | 15-70 ng/dL | Higher (varies) |
| Progesterone | 1-20 ng/mL | Lower (varies) |
| Insulin | 2.6-24.9 µIU/mL | Elevated (varies) |
Knowing these hormone ranges helps spot imbalances early. Early intervention can reduce long-term health risks from PCOS. Treatment plans should include lifestyle changes, diet, and possibly medication. This shows the need for tailored care to improve women’s health with PCOS.
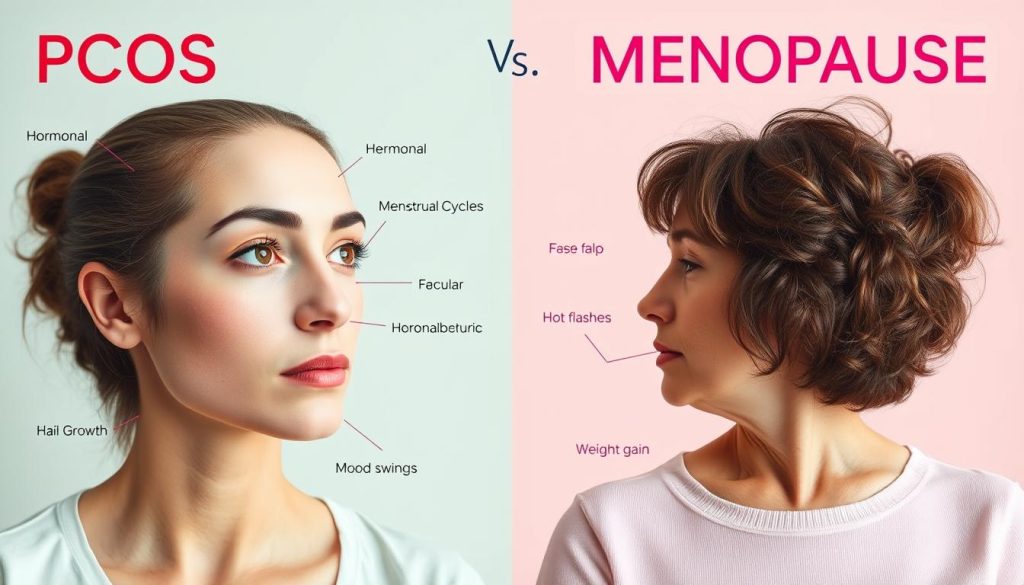
Identifying the Overlap of PCOS and Menopause Symptoms
PCOS (Polycystic Ovary Syndrome) and menopause often share symptoms, making diagnosis tricky. It’s key to understand these overlaps to manage menopausal symptoms and hormonal imbalance effectively.
PCOS and menopause both cause hormonal shifts, leading to similar symptoms. This makes it hard to tell if symptoms come from age or PCOS. It’s a challenge for doctors and patients alike.
- Hot flashes: Both menopause and PCOS patients report hot flashes, though they might start earlier and last longer in individuals with PCOS.
- Mood fluctuations: Hormonal imbalances in PCOS and menopause can cause mood swings, anxiety, and depression.
- Sleep disturbances: Sleep issues like sleep apnea and restless legs syndrome are common in both, due to hormonal changes.
Understanding these shared symptoms helps in finding the right treatment. For example, treatments that balance hormonal imbalance can help with both PCOS and menopause symptoms.
It’s also important to focus on lifestyle changes for both conditions. Changes like diet, exercise, and stress management can help. These actions improve hormonal balance and quality of life for those with PCOS and going through menopause.
Early Signs of Menopause for Women with PCOS
Women with Polycystic Ovary Syndrome (PCOS) often face a unique menopause experience. They need to recognize early signs to manage them well. Knowing early menopause signs helps women prepare for this big change.
Menstrual Irregularities and Changes
One of the first signs of menopause in PCOS women is changes in their periods. These changes, like unpredictable cycles or skipped periods, are due to hormonal shifts. They are different from the usual PCOS symptoms.
Recognizing Perimenopause with PCOS
The time before menopause, called perimenopause, is tough for PCOS women. They might experience sleep issues, mood swings, and changes in sex life. Spotting these early menopause signs early is key to managing them.
Talking to a healthcare provider about PCOS and menopause can help. They can suggest ways to handle menstrual irregularities and other symptoms. This way, women with PCOS can smoothly go through these years.
Managing Hormone Fluctuations During Perimenopause
As women enter perimenopause, keeping hormone levels balanced is key. This helps manage symptoms better. Making lifestyle changes and using hormone therapy can help a lot.
Strategies to Balance Hormones Naturally
There are many ways to keep hormones in check without medicine. Eating right, staying active, and managing stress are effective. A diet full of nutrients and phytoestrogens helps balance hormones.
- Eat foods high in omega-3s like flaxseeds and fish to help with hormone production.
- Regular exercise boosts hormone activity and lowers stress.
- Try yoga and meditation to handle stress and its effects on hormones.
Hormone Replacement Therapy Considerations
Hormone replacement therapy (HRT) is often talked about for perimenopause. It gives hormones to replace those missing after menopause. But, it’s important to think about the benefits and risks for each person.
| Benefits of HRT | Potential Risks of HRT |
|---|---|
| Reduces hot flashes and night sweats | Increase in thrombotic events (e.g., stroke) |
| Improves mood and reduces depressive symptoms | Possible elevated risk of breast cancer |
| Helps in preventing bone loss and fractures | Risk of endometrial cancer if not combined with progesterone |
Choosing hormone therapy should be a team effort with your doctor. Understanding the good and bad points helps tailor the treatment. This makes managing perimenopause better and improves overall health.
PCOS and Menopause: Coping with Hot Flashes and Night Sweats
Women with PCOS and menopause face a tough time with hot flashes and night sweats. These symptoms can disrupt daily life. But, with the right PCOS symptom management, you can lessen their impact. Here are some proven ways to manage these symptoms.
Making lifestyle changes is a key step. Regular exercise and a cool environment at home and work can help. Wearing light, breathable clothes is also a good idea.
- Use cooling gels or moisture-wicking bedding to stay cool at night
- Avoid spicy foods, caffeine, and alcohol to reduce hot flashes
- Try yoga, meditation, or deep-breathing exercises to lower stress
Your diet is also important. Eating a balanced diet with fruits, vegetables, and whole grains can help. It can stabilize blood sugar, which may lessen hot flashes and night sweats.
| Dietary Component | Benefits for PCOS | Benefits for Menopause |
|---|---|---|
| High-fiber foods | Improves blood sugar control and hormonal balance | Helps manage weight and reduces hot flashes |
| Lean proteins | Supports muscle health and balances hormones | Assists in maintaining lean muscle mass during menopause |
| Omega-3 fatty acids | Reduces inflammation and can help with menstrual pain | Improves mood and reduces the frequency of mood swings |
Don’t forget the importance of staying hydrated. It helps manage hot flashes and night sweats. Drinking enough water keeps your body cool from the inside.
If changes in lifestyle and diet don’t help, talk to your healthcare provider. They can discuss medication or hormone therapies for PCOS. Every woman’s experience is different, so getting advice tailored to you is best.
Sexual Health and Intimacy Challenges in PCOS and Menopause
Women with PCOS and menopause face big sexual health and intimacy hurdles. These challenges are tough because of libido changes in PCOS and menopause’s hormonal shifts.
Addressing Libido Changes
Hormonal ups and downs can really affect libido. Libido changes in PCOS often mean less desire. Menopause’s estrogen and progesterone changes make it worse. Doctors say knowing and tackling these changes can help a lot.
Navigating Relationship Dynamics
Hormonal changes affect more than just physical health. They also touch on emotional connection and intimacy in relationships. Relationship counselors stress the need for clear talk and understanding between partners during these times.
| Challenges | Impact on Intimacy | Suggested Strategies |
|---|---|---|
| Libido Changes | Decreased sexual desire | Open communication, seeking medical advice |
| Hormonal Imbalance | Emotional disconnect | Therapy, emotional intimacy exercises |
| Physical Discomfort | Reduced sexual activity | Lifestyle adjustments, lubricants |
It’s key to tackle these intimacy challenges for healthy relationships and overall well-being. With medical and emotional support, women can face these issues with more strength and insight.
Weight Management and Metabolic Health Amidst Hormonal Changes
Managing weight and metabolic health can be tough, more so for women with PCOS and menopause. It’s key to grasp how these conditions affect weight and metabolism. This knowledge helps in creating effective PCOS diets and lifestyle plans.
PCOS, Weight Gain, and Metabolism
PCOS impacts metabolic health, causing weight gain and insulin resistance. Research from The Obesity Society shows PCOS messes with metabolism, making weight control hard. To better metabolic health, women with PCOS should eat more high-quality protein and less high glycemic foods.
Dietary Adjustments for Menopause and PCOS
Diet is vital for managing PCOS and menopause symptoms. Nutrition experts suggest a PCOS diet full of fiber and low in processed foods. This helps control blood sugar and boosts health. Here are some dietary changes to make:
- Eat more whole grains and legumes for fiber.
- Add omega-3s from fish and flax seeds to fight inflammation.
- Lower saturated fats and sugars for better heart health.
| Food Group | Benefits for PCOS | Benefits for Menopause |
|---|---|---|
| Whole Grains | Improves insulin sensitivity | Helps manage weight |
| Lean Proteins | Supports muscle mass | Reduces hot flashes |
| Fruits and Vegetables | Provides necessary vitamins | Enhances mood and energy levels |
Nutritional Needs and Dietary Recommendations for PCOS and Menopause
Women with PCOS and menopause face a tough time with food choices. It’s key to know the nutritional needs for these conditions to stay healthy. This part talks about dietary recommendations backed by science to help those with PCOS and menopause.
Creating a PCOS and menopause diet is more than just food. It’s about how your body uses it. Women with these conditions often struggle with metabolism. So, controlling blood sugar is very important. The diet suggestions here aim to balance hormones, lessen symptoms, and boost overall health.
A diet full of fiber, healthy fats, and lean proteins is essential. It should also be low in processed sugars and unhealthy fats. Here’s a list of foods and habits that can help manage PCOS and menopause:
- High-fiber vegetables like leafy greens and cruciferous vegetables like broccoli and cauliflower.
- Lean protein sources, including chicken, fish, and legumes.
- Healthy fats from avocados, nuts, seeds, and olive oil.
- Whole grains like quinoa, brown rice, and whole oatmeal to help maintain steady blood sugar levels.
| Nutrient | Benefits | Source |
|---|---|---|
| Omega-3 Fatty Acids | Reduce inflammation and support hormonal balance | Fish, flax seeds, walnuts |
| Magnesium | Helps reduce menstrual cramps and improves insulin sensitivity | Dark chocolate, avocados, nuts |
| Fiber | Enhances digestion and aids in sustained blood sugar control | Vegetables, whole grains, legumes |
To follow these dietary tips, planning meals and preparing them in advance is smart. It helps control portions and meet nutritional needs. Focusing on the nutritional needs for a PCOS and menopause diet can greatly improve health and quality of life for women with these conditions.
Mind-Body Approaches to Manage Stress and Emotional Well-being
Using mind-body approaches helps manage stress and boosts emotional health. This is key for women dealing with PCOS and menopause. Experts say these methods combine physical activities with mental health to find effective ways to cope.
The American Psychological Association says meditation and mindfulness are great. They lower stress and improve emotional health. They help manage symptoms of PCOS and menopause. This shows the value of holistic treatments in today’s healthcare.
Beneficial Exercises for PCOS and Menopausal Health
Yoga and tai chi are top choices for mind-body approaches. They improve physical flexibility and strength. They also help with mental focus and mood.
Emotional Support and Counseling
Counseling is vital for emotional support, which is key for managing anxiety and depression with PCOS and menopause. Talking to a therapist helps find personal ways to improve emotional well-being.
| Exercise Type | Benefits | Recommended Frequency |
|---|---|---|
| Yoga | Improves flexibility, reduces stress, aids hormonal balance | 3-4 times a week |
| Tai Chi | Enhances mental focus, increases strength, promotes calmness | 2-3 times a week |
| Meditation | Regulates mood, lowers stress levels, improves sleep quality | Daily |
Medical Treatments and Interventions for PCOS in Menopause
Women with Polycystic Ovary Syndrome (PCOS) may need different treatments as they enter menopause. There are many medical options and surgeries to choose from. Knowing these can help women pick what’s best for them.
Understanding Different Medication Classes
There are many medicines for PCOS symptoms during menopause. Insulin sensitizers like Metformin help with insulin issues. Anti-androgens can also be used to lower male hormones, helping with hair and acne problems.
When Surgery May be Considered
In severe cases, surgery might be needed for PCOS. Procedures like ovarian drilling can help with hormone levels and ovulation. Endometrial ablation can also help with bleeding issues.
It’s important to talk to doctors about treatments for PCOS. They can explain the good and bad of each option. This way, women with PCOS can find the best treatments for their menopause journey.
The Importance of Regular Health Screenings for Women with PCOS
Polycystic Ovary Syndrome (PCOS) is a complex condition that needs constant monitoring. Regular health screenings are key to managing its symptoms and risks. They help in early detection and timely preventive care. This approach improves PCOS management and reduces complications.
Recommended Tests and Check-ups
Health organizations suggest specific tests and check-ups for women with PCOS. These help track health status and check treatment effectiveness.
- Annual physical exams including blood pressure, BMI, and waist measurement evaluations.
- Bi-yearly blood sugar and cholesterol levels to monitor for risks of diabetes and cardiovascular diseases.
- Pelvic ultrasounds to check for ovarian cysts and health.
- Hormonal profile assessments to understand endocrine fluctuations.
Risk Factors and Preventive Care
Understanding PCOS risk factors helps in creating preventive strategies. These strategies can lower the risk of related health issues. Lifestyle changes and medical supervision are essential.
- Maintaining a healthy weight through targeted diet and exercise plans to manage insulin resistance, a key factor in PCOS.
- Regular screenings for mental health to address common issues like depression and anxiety, which are prevalent in PCOS.
- Monitoring inflammation levels, as women with PCOS often exhibit higher systemic inflammatory markers.
Alternative Therapies in the Journey Through PCOS and Menopause
Exploring alternative therapies can open new paths for PCOS treatment and menopause relief. These methods aim for holistic wellness, balancing body and mind. As more people look for non-traditional health solutions, knowing about these treatments is key.
- Acupuncture: Helps restore energy balance, possibly easing hormonal issues in PCOS and menopause.
- Herbal supplements: Used to tackle symptoms like irregular periods and hot flashes.
- Homeopathy: Offers a personalized way to ease symptoms of menopause and PCOS.
Research into these alternative therapies is expanding. It sheds light on their role in PCOS treatment and menopause relief plans. It’s vital to get advice from healthcare experts to safely add these therapies to your routine.
| Therapy Type | Targeted Symptoms | Potential Benefits |
|---|---|---|
| Acupuncture | Hormonal Balance, Hot Flashes | Improves hormonal regulation, reduces frequency of menopause-induced hot flashes |
| Herbal Supplements | Menstrual Irregularity, Mood Swings | Regulates menstrual cycles, stabilizes mood |
| Homeopathy | Sleep Disturbances, Anxiety | Enhances sleep quality, decreases anxiety levels related to menopause and PCOS |
While alternative therapies offer many benefits, it’s important to talk to healthcare providers. They can help create a treatment plan that fits your specific needs and health situation.
Social Support Systems and Communities for Women with PCOS
Women with Polycystic Ovary Syndrome (PCOS) can greatly benefit from the right support systems. PCOS communities and support groups offer a place to share resources and experiences. This can provide emotional and informational support.
Online Resources and Support Groups
Online platforms are key for people facing health challenges. Women with PCOS find a wealth of resources online. This includes medical advice and personal stories of coping with PCOS.
Organizations like the PCOS Awareness Association help make sure reliable information is available. This is a big help for those looking for support.
Online PCOS communities are great because they’re easy to access. Women worldwide can connect and share without needing to be in the same place. This is a big plus for those in areas with few PCOS resources.
Building a Local Support Network
While online forums are helpful, face-to-face interactions are also valuable. Many health centers promote local support networks. These groups meet to talk about PCOS and menopause.
These meetings offer education and social support. They show how important community involvement is in managing PCOS symptoms.
| Support Type | Benefits | Examples |
|---|---|---|
| Online Forums | 24/7 accessibility, wide range of information, anonymity | PCOS Awareness Association webinars, Facebook groups |
| Local Support Groups | Personal connection, immediate emotional support, community engagement | Community health center workshops, local PCOS support meetups |
Real-life Stories: Coping Strategies from Women with PCOS and Menopause
Real-life stories of PCOS and menopause are more than just tales. They offer wisdom to those on similar paths. Health blogs and memoirs share many coping strategies. These range from diet changes to managing daily routines.
These personal stories highlight the importance of maintaining quality of life. They show how to deal with hormone changes and their effects. Women share tips on planning, using supplements, and making lifestyle changes.
They talk about yoga and meditation for mental health. Regular exercise is also key for mood and anxiety. Reflecting on menopause, listening to your body is vital. Talking to doctors and finding support groups are also important.
These stories do more than inform; they empower. They give others the tools to manage PCOS and menopause. Embracing these stories helps us stay hopeful and proactive about our health.
FAQ
Q: What is Polycystic Ovary Syndrome (PCOS)?
A: PCOS is a hormonal disorder that affects many women of childbearing age. It can cause irregular periods and high levels of male hormones. The ovaries may also have many small fluid collections and not release eggs regularly.
Q: How does PCOS affect women’s long-term health?
A: PCOS can lead to serious health issues like diabetes and heart disease. It also raises the risk of high blood pressure, sleep apnea, and depression. Women with PCOS should manage their condition to avoid these risks through lifestyle changes and medical care.
Q: Can PCOS cause hormonal imbalance?
A: Yes, PCOS leads to hormonal imbalances. This can include high male hormone levels and insulin resistance. It can also affect the menstrual cycle, causing infertility, acne, and abnormal hair growth.
Q: Are menopausal symptoms similar to PCOS symptoms?
A: Menopause and PCOS share symptoms like hot flashes and mood swings. But, they have different causes. Each condition needs its own management plan.
Q: What are early signs of menopause for women with PCOS?
A: Women with PCOS may notice changes in their periods, like irregular or missed periods. These changes can be signs of both PCOS and menopause. It can be hard to tell them apart.
Q: How can hormone fluctuations be managed during perimenopause for those with PCOS?
A: Managing hormone changes in perimenopause involves lifestyle changes. Eating well, exercising, and getting enough sleep are key. Hormone Replacement Therapy (HRT) might also be an option, but it should be discussed with a doctor.
Q: What are effective ways to cope with hot flashes and night sweats in PCOS and menopause?
A: To deal with hot flashes and night sweats, keep your bedroom cool. Avoid spicy foods and caffeine. Wear breathable clothes and use cooling products. Staying hydrated and managing stress can also help.
Q: How can women navigate changes in libido and intimacy during PCOS and menopause?
A: Women can talk openly with their partners about changes in libido. Seeking counseling and exploring therapies can help. Doctors may suggest treatments like vaginal lubricants or estrogen to improve sexual health.
Q: What dietary adjustments can help with weight management during PCOS and menopause?
A: For weight management, focus on whole foods and increase fiber. Avoid processed foods and sugars. Monitor carbs to control blood sugar. A nutritionist can offer personalized advice.
Q: What kinds of exercises are beneficial during PCOS and menopausal health?
A: Good exercises for PCOS and menopause include cardio, strength training, and yoga. These improve metabolism and reduce stress. Tailor your routine to your health and preferences.
Q: Are there alternative therapies for treating symptoms of PCOS and menopause?
A: Yes, alternative therapies like acupuncture and herbal supplements may help. But, always talk to a doctor first. They should be used safely with medical treatments.
Q: What social supports exist for women with PCOS?
A: Women with PCOS can find support online, in support groups, and at health centers. These places offer a space to share experiences and find resources.