Getting a stage 3 breast cancer diagnosis can feel overwhelming. It’s a scary time filled with uncertainty. It’s the start of a long journey, where you’ll need to learn about your treatment options and what’s ahead.
Knowing about your cancer is key. It’s not just about following doctor’s orders. It’s about taking control of your health and facing the challenges ahead.
Understanding stage 3 breast cancer is just the beginning. It’s a long journey many people face. With the right knowledge and support, you can make choices that affect your treatment and recovery.
This guide will help you cope with your diagnosis. It will also give you the basic knowledge you need for the journey ahead.
Key Takeaways
- Stage 3 breast cancer diagnosis marks a critical point in the patient journey, requiring comprehensive understanding and support.
- Treatment considerations at this stage are highly personalized and demand a clear grasp of the disease’s specifics.
- Being informed about your condition empowers you to make decisions that best suit your individual health needs.
- Emotional support and resources are just as crucial as medical treatment in managing the impact of your diagnosis.
- Understanding your diagnosis is the first step in formulating a treatment plan tailored to your unique situation.
What is Stage 3 Breast Cancer?
Stage 3 breast cancer, also known as locally advanced breast cancer, is a serious stage. It’s different from earlier stages because of its size, lymph node involvement, and spread. This stage is key to understanding the aggressive nature of invasive breast carcinoma and planning effective treatments.
This stage is divided into subcategories (IIIA, IIIB, and IIIC). Each subcategory shows specific details about tumor size and lymph node involvement. For example, Stage IIIC means cancer has spread to lymph nodes near the collarbone or internal mammary glands, no matter the tumor size.
Understanding stage 3 breast cancer is crucial for creating treatment plans. These plans address the disease spread and aim to improve treatment outcomes.
- A tumor larger than 5 cm or smaller tumors with multiple lymph nodes.
- Cancer extending to the chest wall or skin of the breast, including inflammatory breast cancer.
- Significant lymph node involvement, possibly in the underarm, collarbone, or internal regions near the breast.
The treatment outlook for stage 3 breast cancer includes a mix of therapies. These aim to reduce the chance of metastasis and improve survival. Treatments may include surgery, chemotherapy, radiation therapy, and targeted biological therapies. This comprehensive approach targets locally advanced breast cancer.
| Substage | Tumor Size | Lymph Node Involvement | Common Treatments |
|---|---|---|---|
| IIIA | <5 cm | 4-9 nodes | Chemotherapy, Surgery |
| IIIB | Variable, may invade skin | Extensive regional | Radiation, Targeted therapy |
| IIIC | May be any size, often larger | Near collarbone, mammary | Comprehensive multimodal treatment |
Understanding invasive breast carcinoma in this advanced stage helps patients and caregivers. It makes it easier to navigate treatment options and manage the condition.
The Different Subtypes of Stage 3 Breast Cancer
Knowing the subtypes of Stage 3 breast cancer is key for finding the right treatment strategies and understanding the prognosis. Each subtype has its own challenges, affecting how we treat and what the outcome might be for patients.
Talking about early prevention strategies and regular health checks can help manage these subtypes well.
Invasive Breast Carcinoma
Invasive breast carcinoma means cancer cells have spread into the surrounding breast tissue. This type is very aggressive and needs a detailed treatment plan to control its growth and improve patient results.
Locally Advanced Breast Cancer
Locally advanced breast cancer means tumors have grown to nearby areas like skin, muscle, or lymph nodes but not to distant organs. It’s crucial to have a treatment plan that focuses on both controlling the disease locally and using systemic therapies to stop it from coming back.
Node-Positive Breast Cancer
Node-positive breast cancer is when cancer cells are found in the lymph nodes near the breast. This often means more intense treatments are needed because of the higher risk of spreading, which greatly affects the prognosis.
Understanding these subtypes helps in creating treatment strategies that fit each patient’s needs. This can greatly improve the prognosis for those with Stage 3 breast cancer.
Stage 3 Breast Cancer: Treatment Options
Treatment for stage 3 breast cancer needs a multidisciplinary approach. This means a team of experts like oncologists, surgeons, and radiologists work together. They create a personalized treatment plan that fits the patient’s needs and health.
This plan makes sure the breast cancer therapy is both thorough and focused on the patient.
There are many treatment options for stage 3 breast cancer. These include new therapies being tested in clinical trials. The main treatments are:
- Surgery (lumpectomy, mastectomy)
- Chemotherapy
- Radiation therapy
- Hormonal treatments (if cancer is hormone receptor-positive)
- Targeted therapies (depending on the cancer’s specific characteristics)
Each treatment is chosen based on how well it works against the tumor’s unique traits. For example, targeted therapies are picked based on genetic tests. This helps tailor the treatment to the cancer’s specific mutations.
| Treatment Type | Considerations | Common Approaches |
|---|---|---|
| Surgery | Extent of cancer spread, patient health | Mastectomy, Lumpectomy |
| Chemotherapy | Cancer’s responsiveness, prior treatments | Neoadjuvant, Adjuvant |
| Radiation Therapy | Location of tumor, post-surgical considerations | External beam radiation, Brachytherapy |
| Targeted Therapy | Genetic markers, previous response to treatments | HER2 inhibitors, PARP inhibitors |
Creating an effective personalized treatment plan also means regular checks to see how it’s working. This allows for changes to the treatment as needed. This approach helps improve results and manage side effects better.
In conclusion, using a multidisciplinary approach helps create treatment plans that are tailored to each patient. This shows how complex stage 3 breast cancer is. It also highlights the need for treatments that are as unique as the people they help.
Factors Affecting Stage 3 Breast Cancer Prognosis
Understanding Stage 3 breast cancer means looking into key prognosis factors. These include the cancer’s subtype and the receptor status. These factors greatly affect how well the cancer responds to treatment.
HER2-Positive Breast Cancer
HER2-positive breast cancer has too much of the HER2 protein. This makes it grow fast. But, the right treatment can help slow it down and improve the outlook.
Triple-Negative Breast Cancer
Triple-negative breast cancer doesn’t have receptors for hormones or HER2. It’s hard to treat because it doesn’t respond to hormone therapy. Knowing this is key to understanding treatment options.
Hormone Receptor-Positive Breast Cancer
Breast cancer with hormone receptors can be treated with hormone-blocking drugs. This type of cancer often has a better chance of being treated successfully. It shows how important the receptor status is.
| Cancer Subtype | Treatment Response | Prognosis Factor |
|---|---|---|
| HER2-Positive | Highly responsive to targeted therapies | Dependent on prompt and precise treatment |
| Triple-Negative | Less responsive to hormonal therapies | Generally more aggressive with varying outcomes |
| Hormone Receptor-Positive | Responsive to hormone-blocking agents | Typically more favorable outcome |

The Role of Surgery in Treating Stage 3 Breast Cancer
Surgery is key in treating stage 3 breast cancer. This article looks at the surgical options like lumpectomy, mastectomy, and reconstructive surgery. It explains the goals and what to expect from each.
Finding the right surgery is crucial. It’s important to talk to your care team about the pros and cons of each option.
- Lumpectomy: This is often chosen when the cancer is small. It removes the tumor and a bit of tissue around it, keeping most of the breast.
- Mastectomy: This is needed if there are big tumors or a high risk of cancer coming back. You might choose to remove one or both breasts. This choice depends on many factors, like your genes.
- Reconstructive Surgery: After a mastectomy, many choose to have their breasts rebuilt. You can use implants or take tissue from another part of your body. This choice can greatly affect how you feel after surgery.
Choosing surgery is a personal decision. It depends on your health, how you feel about your body, and your mental well-being.
Choosing the right surgery means understanding what to expect and possible risks. You should talk about survival rates and how you’ll feel after surgery. This includes how you’ll feel about your body, sex life, and any physical changes.
Getting help from many doctors and mental health experts is helpful. They make sure you get all the care you need to recover well.
Chemotherapy and Radiation Therapy
Neoadjuvant chemotherapy and adjuvant therapy are key in treating stage 3 breast cancer. They target cancer cells at important times. Radiation treatment also plays a big role in getting rid of cancer cells left after surgery.

Neoadjuvant chemotherapy is given before surgery to make the tumor smaller. This makes surgery easier or less invasive. It helps kill more cancer cells, improving surgery results and chances of recovery.
Adjuvant therapy is used after surgery to kill any cancer cells left behind. It’s vital in lowering the chance of cancer coming back. Chemotherapy can include different drugs based on the cancer type and the patient’s health.
- Radiation treatment comes after surgery and chemotherapy, especially if there’s a high risk of cancer coming back.
- Its goal is to kill any cancer cells left behind. It targets the chest wall and lymph nodes to cover all areas at risk.
The success of radiation therapy depends on the right timing and dosage for each patient. It’s a personalized part of cancer treatment.
This integrated approach ensures a multi-disciplinary strategy in combating stage 3 breast cancer, significantly improving patient outcomes.
Targeted Therapies for Stage 3 Breast Cancer
In the fight against stage 3 breast cancer, targeted therapy is making a big difference. It uses monoclonal antibodies and signal transduction inhibitors to attack cancer cells directly. This new approach is a big change from old treatments, offering treatments that fit each person’s cancer.
Monoclonal Antibodies
Monoclonal antibodies are a key part of targeted therapy. They go straight for cancer cells, leaving healthy cells alone. This makes treatments work better and have fewer side effects.
Signal Transduction Inhibitors
These drugs block proteins that help cancer cells grow. By stopping these signals, they stop cancer cells from growing and spreading. This is a targeted way to slow down the disease.
Adding these therapies to treatment plans for stage 3 breast cancer is showing great results. Patients are living longer without their cancer getting worse.
| Treatment Type | Function | Common Drugs |
|---|---|---|
| Monoclonal Antibodies | Targets and destroys cancer cells | Trastuzumab, Pertuzumab |
| Signal Transduction Inhibitors | Blocks growth signals in cancer cells | Lapatinib, Everolimus |
The table shows how these targeted therapies work to stop cancer cells from living. They give hope and a second chance to many patients with this tough cancer.
Hormonal Therapies for Hormone Receptor-Positive Stage 3 Breast Cancer
For those with stage 3 breast cancer that’s hormone receptor-positive, hormone therapy is key. The presence of estrogen receptors and progesterone receptors on cancer cells guides treatment. These therapies block estrogen’s effect on breast cancer, slowing tumor growth and lowering recurrence risk.

Drugs like Tamoxifen and Toremifene block estrogen receptors. Fulvestrant degrades these receptors. It’s crucial to understand how these drugs interact with receptors for effective treatment.
Suppressing estrogen’s influence is central to hormonal therapy. This hormone can fuel cancer cell growth. Hormonal therapies also include aromatase inhibitors and ovarian suppression for pre-menopausal women. Aromatase inhibitors cut estrogen production in postmenopausal women, further reducing hormone levels that can fuel cancer.
- Tamoxifen: Blocks the estrogen from connecting to the estrogen receptor on cancer cells.
- Fulvestrant: Degrades the estrogen receptor, thus preventing its activation.
- Aromatase Inhibitors: Lowers estrogen levels by inhibiting the aromatase enzyme.
- Ovarian Suppression: Reduces estrogen levels by temporarily stopping ovary function.
Patients often face side effects from hormonal changes. This shows the need for support and careful monitoring during treatment. Treatment plans must consider the cancer’s characteristics, the patient’s health, and how they metabolize hormones.
Hormone therapy is a vital part of treating hormone receptor-positive stage 3 breast cancer. It’s effective in reducing recurrence and is used after surgery or chemotherapy. This highlights the importance of understanding breast cancer biology and treatment mechanisms.
Understanding Inflammatory Breast Cancer
Inflammatory breast cancer is a very aggressive cancer type in breast cancers. It doesn’t show up as a lump like other cancers. This makes it hard to diagnose early, which is why knowing the symptoms is key.
The main symptoms include fast swelling and redness of the breast. The skin might look like an orange peel. The breast can also feel warmer and heavier, with pain or the nipple turning inward.
Doctors use physical exams, imaging tests, and biopsies to diagnose. Treatments are strong because of the cancer’s fast growth. They often start with chemotherapy, then surgery and radiation.
- Swelling and redness of the breast
- Orange peel texture of the skin
- Increased warmth and heaviness in the affected breast
- Pain and changes to the nipple’s appearance
Spreading the word about inflammatory breast cancer can help a lot. If you see these symptoms, get medical help right away. Early detection is crucial for treatment success.
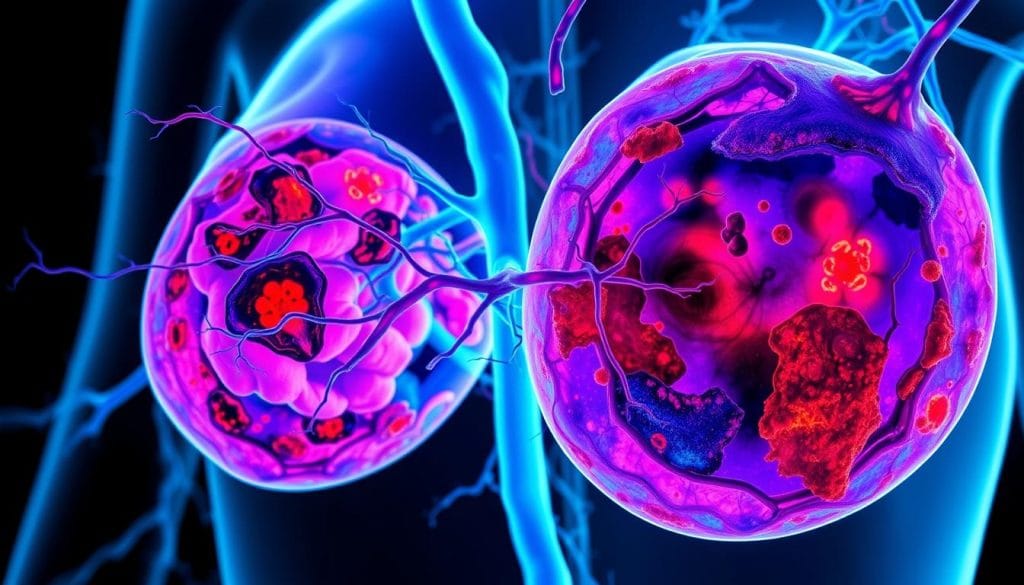
The Impact of Metastatic Spread in Stage 3 Cancer
Understanding how stage 3 breast cancer spreads is key to managing it well. This stage can involve locoregional spread and distant metastasis. These factors greatly affect treatment plans.
Metastatic breast cancer means the cancer has spread to other parts of the body. It can go to nearby lymph nodes (locoregional spread) or distant organs like the lungs or bones (distant metastasis). Each spread type changes treatment options and outlook.
- Locoregional Spread: Cancer cells move to nearby lymph nodes or tissues, usually first.
- Distant Metastasis: Cancer cells travel far from the original tumor, making treatment harder.
Knowing the difference between locoregional and distant metastasis is crucial for treatment planning. Treatments can range from surgery and radiation to chemotherapy and targeted therapies. This depends on how far and where the cancer has spread.
When cancer spreads differently, treatments must change. Here’s a look at typical treatments for each spread type:
| Treatment Approach | Locoregional Spread | Distant Metastasis |
|---|---|---|
| Surgery and Radiation | Often enough | Used to ease symptoms |
| Systemic Therapy | May be needed | Usually required |
| Prognostic Impact | Usually better | Can be tough |
Knowing if metastatic breast cancer has spread locally or distantly is crucial. It affects both the disease’s outlook and its management. So, treatment plans must be regularly checked and updated to keep up with the cancer’s changing nature.
Navigating Stage 3 Breast Cancer with Breast Conservation Therapy
Breast conservation therapy is a big choice for stage 3 breast cancer patients. It uses lumpectomy and radiation therapy to remove cancer while keeping more of the breast. Knowing about this treatment helps patients make better health care choices.
Lumpectomy is a key part of this therapy. It removes the tumor and a bit of tissue around it. This is different from mastectomy, which removes the whole breast. After lumpectomy, radiation therapy is used to kill any cancer cells left behind.
Choosing breast conservation therapy depends on many things. These include tumor size, location, genetics, and personal wishes. Let’s look at the benefits and downsides of this therapy:
| Treatment Approach | Benefits | Considerations |
|---|---|---|
| Breast Conservation Therapy | Possible retention of breast appearance and sensation, shorter recovery periods | May require follow-up treatments; careful patient monitoring essential |
| Mastectomy | Greater assurance of cancer removal | Longer recovery periods, potential need for reconstructive surgery |
By comparing these options, patients can talk better with their oncologists. This helps choose a treatment that fits their health goals and lifestyle.
In the end, breast conservation therapy tries to treat cancer well while keeping quality of life in mind. It’s a good option for stage 3 breast cancer. Talking to healthcare providers about this therapy can help understand how it fits into your cancer care plan.
Evaluating the Risks and Benefits of Mastectomy
Choosing to have a mastectomy for stage 3 breast cancer is a big decision. It’s about weighing the good and bad sides of the surgery. This part will help you understand what to think about before making a choice.
Mastectomy benefits might include getting rid of most cancer cells. This could lower the risk of cancer coming back in the breast. But, like any big surgery, there are risks and possible problems to think about carefully.
“Understanding both the risks and benefits is essential in making an empowered decision that aligns with one’s health goals and personal circumstances.”
Factors Influencing the Decision:
- Evaluation of Personal and Family Medical History: Looking into your family’s health and your own health history.
- Risks Associated with Surgery: This includes immediate risks and long-term effects like lymphedema or other complications.
- Post-Surgical Recovery: Thinking about how long it takes to get better and the physical and emotional effects.
- Alternative Treatments: Looking at other treatments that might work with or instead of mastectomy, based on your tumor and what you prefer.

The Table below shows the good and bad sides of mastectomy. It’s a quick guide for making a decision.
| Benefits of Mastectomy | Possible Surgical Risks |
|---|---|
| Reduces the chance of breast cancer recurrence | Postoperative infection |
| Can aid in improving overall prognosis | Complications such as bleeding or anesthesia-related issues |
| Eliminates the need for frequent monitoring of breast changes | Possible long-term physical changes impacting body image and emotional health |
Deciding on mastectomy is complex. It’s not just about the good and bad sides of surgery. You also need a strong support system to help you make this choice. Talking to doctors, looking at the latest research, and thinking about your health goals are key steps.
The Importance of Lymph Node Analysis
In the world of breast cancer, knowing about lymph nodes is key. Sentinel lymph node biopsy and lymph node dissection are vital for cancer staging. This step is crucial for deciding treatment and predicting outcomes.
Sentinel lymph node biopsy shows if cancer has spread early. It helps avoid removing too many lymph nodes. This reduces risks like lymphedema and gives vital info for treatment plans.
Lymph node dissection is needed when sentinel nodes show cancer. It removes many nodes for a closer look. This helps figure out how far cancer has spread, guiding treatment.
The results of these tests are key to correct cancer staging. They help create treatment plans that fit each patient’s needs. Knowing about lymph node analysis helps those facing stage 3 breast cancer.
Lifestyle and Supportive Care during Stage 3 Breast Cancer Treatment
Dealing with Stage 3 breast cancer is tough. It’s important to focus on physical and mental health. Having a strong support system is key too. These efforts improve life quality and are part of survivorship care.
Nutrition and Exercise
Eating right and staying active are crucial. A healthy diet boosts the immune system and helps with treatment side effects. Exercise is also important for heart health, weight management, and mood.
Mental Health Support
Mental health is a big part of cancer care. The journey can be hard on the mind. Counseling and support groups help manage emotional stress, improving life quality.
Social Support and Resources
A strong support network is essential. Family, friends, and groups offer mental and physical support. Educational resources and community programs help patients manage their condition.
Conclusion
Dealing with stage 3 breast cancer is a tough journey. It’s filled with uncertainty and challenges. But, we’ve tried to help by explaining the details of different types and treatment options. Our goal is to empower you with knowledge.
Knowing a lot about your cancer helps you talk better with doctors. It also leads to treatments that fit you best. This knowledge is a powerful tool in your fight against cancer.
There’s also hope in new treatments that are getting better all the time. These advancements help doctors find and fight cancer cells better. They also try to protect healthy parts of your body.
These scientific steps give patients and their families a positive outlook. They show that there’s always a chance for a better future.
But, there’s more than just treatments. There’s also a strong support network to help you. Taking care of your emotional health, eating right, and finding community help are all key. You’re not alone in this fight.
Every step you take towards awareness, treatment, and support is brave. It shows courage, hope, and strength. Keep moving forward, knowing you have a supportive community behind you.
FAQ
What exactly is Stage 3 Breast Cancer?
Stage 3 breast cancer is a more advanced form of the disease. The tumor may be over five centimeters or have spread to lymph nodes. It can also reach the chest wall or skin of the breast.
It’s divided into stages 3A, 3B, and 3C. These depend on the tumor size and how far it has spread.
Can you explain the different subtypes of Stage 3 Breast Cancer?
Stage 3 breast cancer has different subtypes. These include invasive breast carcinoma and locally advanced breast cancer. Each subtype has its own features that affect treatment and prognosis.
For example, how much the tumor has spread and whether it involves lymph nodes.
What are the treatment options for Stage 3 Breast Cancer?
Treatment for Stage 3 breast cancer is a mix of surgery, chemotherapy, and radiation therapy. The goal is to create a treatment plan that fits each patient’s needs.
How does the cancer subtype affect the prognosis of Stage 3 Breast Cancer?
The subtype of breast cancer greatly affects prognosis. For instance, HER2-positive cancers may respond well to targeted therapies. Triple-negative cancers are harder to treat.
Hormone receptor-positive cancers can be treated with hormone-blocking drugs. The subtype determines the treatment approach and outcomes.
What surgical options are available for treating Stage 3 Breast Cancer?
Surgical options include lumpectomy and mastectomy. Lumpectomy removes the tumor and some tissue. Mastectomy removes the whole breast.
Reconstructive surgery may follow mastectomy. The choice depends on the tumor size, location, patient preference, and overall health.
Can you explain the role of chemotherapy and radiation therapy in treating Stage 3 Breast Cancer?
Chemotherapy is given before or after surgery. It aims to shrink the tumor or eliminate remaining cancer cells. Radiation therapy is used after surgery to destroy any cancer cells left behind.
It’s especially important for breast conservation therapy to preserve the breast.
What advancements are there in targeted therapies for Stage 3 Breast Cancer?
Targeted therapies, like monoclonal antibodies, block molecules involved in cancer growth. For example, trastuzumab targets HER2-positive breast cancer cells. These therapies improve outcomes for certain subtypes.
How do hormonal therapies work for Hormone Receptor-Positive Stage 3 Breast Cancer?
Hormonal therapies target estrogen and progesterone receptors on hormone receptor-positive breast cancer cells. Drugs like tamoxifen block these receptors or lower hormone levels. This reduces cancer cell growth and survival.
What makes Inflammatory Breast Cancer distinct from other types of Stage 3 Breast Cancer?
Inflammatory breast cancer is rare and aggressive. It causes redness, swelling, and dimpling of the breast skin. It grows quickly and often spreads to lymph nodes.
Prompt and aggressive treatment is critical due to its rapid progression.
What implications does metastatic spread have on Stage 3 Breast Cancer treatment?
Stage 3 breast cancer involves significant spread to surrounding tissues or lymph nodes. Treatment aims to control this spread and remove or destroy the cancer locally. If cancer has spread to distant parts of the body, more comprehensive treatment is needed.
What is Breast Conservation Therapy?
Breast conservation therapy involves a lumpectomy followed by radiation therapy. It aims to treat the cancer while preserving the breast. It’s an option for some women with Stage 3 breast cancer, depending on the tumor size and location.
What are the risks and benefits of a mastectomy for Stage 3 Breast Cancer?
Mastectomy is often recommended for larger or more aggressive tumors. It removes as much cancerous tissue as possible, potentially reducing recurrence risk. Risks include surgical complications, recovery time, impact on body image, and the need for additional treatments.
Why is lymph node analysis important in treating Stage 3 Breast Cancer?
Lymph node analysis helps determine if cancer has spread to the lymphatic system. It’s crucial for staging, guiding treatment, and providing a prognosis. Procedures like sentinel lymph node biopsy or lymph node dissection are used.
What are the important aspects of supportive care during Stage 3 Breast Cancer treatment?
Supportive care includes a healthy diet and exercise routine to manage side effects and improve recovery. Mental health support, like counseling or support groups, is vital for emotional well-being. Social support and resources like financial assistance and patient education also impact quality of life.