Dealing with a stage 4 pressure wound is a big challenge. It needs special care and attention. This guide is here to help with the latest on healing pressure sores.
It’s based on the newest medical advice and best practices for advanced pressure injury care. The right treatment is key for recovery and a better life. This guide is for healthcare workers, caregivers, and patients. It shines a light on the way to heal and overcome these serious injuries.
Understanding Stage 4 Pressure Wounds
A Stage 4 pressure ulcer is very severe. It causes skin loss and damages muscles, bones, or other structures. These injuries need quick and detailed care to avoid serious problems.
Defining Stage 4 Pressure Ulcers
The National Pressure Ulcer Advisory Panel (NPUAP) says a fourth degree pressure ulcer is very deep. It goes through the skin to muscle or bone. This can lead to serious infections and more problems.
The Severity of a Deep Tissue Injury
A deep tissue injury starts with skin that looks fine but later turns into an open wound. It’s hard to spot early and can get worse fast if not treated.
Recognizing the Signs and Symptoms
Signs of a critical pressure ulcer include deep wounds, exposed bones or tendons, and discolored or black tissue. These signs mean the wound is very serious and needs immediate doctor’s care.
| Attribute | Characteristic of Stage 4 Pressure Ulcer | Characteristic of Less Severe Wound |
|---|---|---|
| Depth | Exposure of bones, muscles | Primarily affects skin layers |
| Signs | Bone visibility, sever infection risk | Mild discoloration, minimum tissue loss |
| Risk Level | High risk for severe infection and complications | Lower risk, more responsive to initial treatment stages |
This detailed look shows how important it is to treat stage 4 pressure ulcers quickly and with the right care. This helps prevent the situation from getting worse.
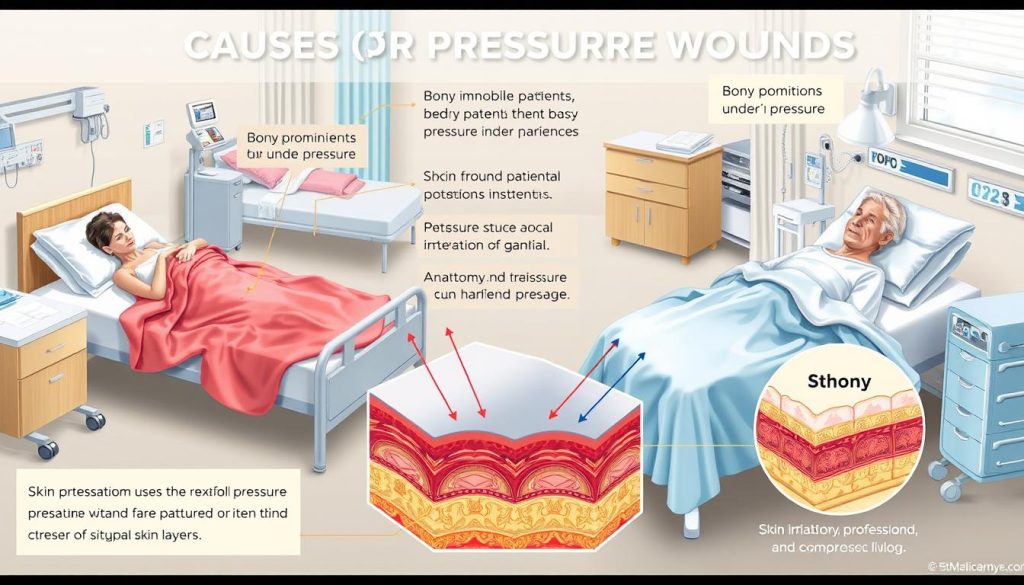
Key Causes and Risk Factors for Advanced Pressure Injuries
Knowing the main pressure wound causes and spotting pressure ulcer stage 4 risk factors is key to stopping and handling these serious issues. Many studies and expert opinions have found certain factors that greatly help in creating advanced stage pressure injuries.
Being stuck in one place for too long can greatly raise the chance of getting a stage 4 bed sore. People who can’t move on their own because of health issues or after big surgeries are at a higher risk. This lack of movement puts constant pressure on some areas of the body. If this pressure doesn’t get relieved, it can cut off blood flow and start to damage the skin and tissues underneath.
- Limited mobility or complete immobility
- Inadequate nutrition and hydration
- Moisture from sweating or incontinence
- Decreased sensory perception in patients with spinal injuries or neuropathy
Not getting enough nutrients is also a big pressure ulcer stage 4 risk factor. Not having enough proteins, vitamins, and minerals can make the skin weak and harder for it to heal. This makes it more likely to get pressure wounds.
Here’s a closer look at what makes stage 4 bed sore risks higher:
| Factor | Impact |
|---|---|
| Prolonged Immobility | Leads to sustained pressure on skin, impairing blood flow and tissue viability |
| Nutritional Deficiencies | Compromises skin integrity and delays healing processes |
| Moisture and Incontinence | Increases skin’s susceptibility to breakdown and infection |
| Age and Chronic Conditions | Affects skin elasticity and overall health status, increasing fragility |
It’s very important for those taking care of others and healthcare workers to watch these risk factors closely. They need to take steps to prevent severe pressure ulcers from happening.
Comprehensive Assessment of a Stage 4 Pressure Wound
Checking stage 4 pressure wounds carefully is key for good care. The right checks help doctors find the right treatment. They also guide on how to get better.
Importance of Accurate Diagnosis
Getting a accurate pressure wound diagnosis is the first step in treating severe ulcers. Knowing the wound’s size and any hidden problems helps start treatment fast. The Wound, Ostomy and Continence Nurses Society says it’s important to know which tissues are affected to choose the right treatment.
Tools and Techniques for Assessing Severe Pressure Sores
New tech has made checking critical pressure ulcers better. Doctors now use high-tech images to see deep into wounds. This helps find hidden infections and plan better treatments.
When to Consult a Wound Care Specialist
Knowing when to see a wound care specialist is very important. You might need one if the wound doesn’t get better or shows signs of infection. Specialists bring new ideas for care that can help a lot.
Principles of Managing a Critical Pressure Ulcer
Managing severe pressure sores, like stage 4, needs strict stage 4 pressure wound care principles. These rules help ease the wound’s severe state. They also promote healing and stop more problems.
Managing severe pressure sores needs a team effort. This ensures all aspects of care are covered. It includes regular checks, special treatments, and watching the wound closely to change the plan as needed.
- Timely and proper wound cleaning to lower infection risks.
- Advanced dressings to keep the wound moist.
- Pressure relief methods like special mattresses and moving schedules.
- Good nutrition to help the skin heal.
Knowing and using these stage 4 pressure wound care principles is key for treating serious ulcers. For more information and a detailed look at managing severe pressure sores, check out this guide.
Wound Cleaning and Care Techniques
Managing stage 4 pressure wounds requires careful cleaning and dressing. It’s important to keep the wound area clean and moist. This helps prevent infections and promotes healing.
Proper Wound Cleaning Protocols
Cleaning wounds for pressure sores is not just about rinsing. It’s about removing dirt while keeping healthy tissue safe. Saline solutions are good for cleaning without harming the wound.
Selecting the Right Dressings and Bandages
Choosing the right dressings is key to healing. Hydrocolloid, foam, and alginate dressings are best. They keep the wound moist, which helps it heal faster.
| Dressing Type | Properties | Best Use |
|---|---|---|
| Hydrocolloid | Moisture-retentive, self-adhesive | Wounds with mild to moderate exudate |
| Foam | High absorbency, padding effect | Highly exudative wounds, protection |
| Alginate | Fiber dressing, highly absorbent | Deep, wet wounds with significant drainage |
Keeping the Wound Environment Optimal for Healing
It’s important to keep the wound area balanced in moisture and temperature. Using advanced wound care products helps. They keep the wound moist, speeding up healing.
Infection Prevention and Control Measures
Managing stage 4 pressure wounds requires a key strategy: preventing infection in pressure ulcers. Proper infection control for stage 4 bed sores is vital for patient recovery. Healthcare experts recommend several essential steps to prevent and control infections effectively.
- Regular Inspection and Cleansing: It’s important to check and clean the ulcer often to stop contamination and infection.
- Use of Antimicrobials: Using topical antimicrobials or antiseptic agents as advised by doctors can reduce bacteria.
- Moisture Management: Keeping the wound moist but not too wet is key to stopping bacteria growth, helping prevent infection in pressure ulcers.
- Comprehensive Hygiene: Good hygiene for the patient and their care environment is critical for infection control for stage 4 bed sores.
Monitoring the wound closely is vital. Regular checks help adjust care plans as the wound changes. Here’s a table showing important supplies and their roles in preventing infections in stage 4 pressure ulcers:
| Supply | Application | Function |
|---|---|---|
| Hydrocolloid Dressings | Wound Covering | Maintains moisture, supports healing |
| Saline Solution | Cleansing Agent | Helps in gentle cleansing without irritation |
| Medical Gloves | Personal Protection | Prevents cross-contamination |
| Barrier Creams | Skin Protection | Prevents excess moisture and bacterial growth |
This approach ensures each care step, from cleaning to protection, focuses on preventing infection in pressure ulcers. It greatly helps in infection control for stage 4 bed sores.
Nutritional Support and Management for Wound Healing
Good wound care is more than just medical treatments and dressings. It also includes a lot of nutritional support. Eating the right foods is key to helping wounds heal faster and better. This part will talk about the best foods and nutrients for quick and effective healing.
The Role of Nutrition in Tissue Repair
Good nutrition is very important for healing wounds. It helps the body fix damaged tissues. Eating enough protein, carbs, and fats can really help wounds heal faster and better.
Essential Vitamins and Minerals for Skin Integrity
Vitamins and minerals are very important for keeping the skin healthy. They help with collagen, fighting off infections, and reducing swelling. Foods rich in Vitamin C, Zinc, and Vitamin A are very helpful for skin health, which is key for managing wounds.
Dietary Adjustments to Support Recovery
Changing your diet can really help with healing stage 4 pressure sores. Dietary management for pressure wounds should include more calories and nutrients for skin repair. Here are some food tips to help wounds close and improve overall health.
| Nutrient | Sources | Benefits |
|---|---|---|
| Protein | Chicken, Fish, Dairy, Beans | Supports cell repair and growth |
| Vitamin C | Citrus Fruits, Peppers, Greens | Promotes collagen formation |
| Zinc | Nuts, Whole Grains, Seafood | Boosts immune function |
| Vitamin A | Carrots, Sweet Potatoes, Spinach | Improves skin integrity |
Pain Management Strategies for Stage 4 Bed Sores
Managing pain from pressure ulcers requires both medicine and non-medical methods. This ensures patients are comfortable and can heal. Stage 4 bed sores are very painful, so a special plan to relieve pain from severe pressure sores is key.
- Topical analgesics help reduce pain right at the sore.
- Doctors may give systemic pain relievers like NSAIDs or opioids for severe pain.
- Changing positions often helps avoid pressure spots and improves blood flow.
- Using advanced mattresses like air-fluidized beds can spread out pressure and lessen pain.
Adding relaxation and distraction methods can also help with pain management for pressure ulcers. These include:
- Guided imagery or relaxation exercises to calm the mind.
- Music or art therapy to take the mind off the pain.
| Treatment Type | Description | Benefit |
|---|---|---|
| Topical Medications | Application of local anesthetics | Direct pain relief at the sore spot |
| Systemic Medications | Oral or IV pain relievers | Addresses widespread body pain |
| Physical Interventions | Repositioning and specialized mattresses | Helps in relieving pressure and improving blood flow |
| Psychological Methods | Guided imagery, music, and art therapy | Aids in mental well-being, reducing perception of pain |
The aim of these methods is not just to relieve pain from severe pressure sores. It’s also to help patients recover fully and improve their quality of life.
Debridement Options for Stage 4 Pressure Wounds
Knowing the different debridement methods is key to treating stage 4 pressure wounds. These wounds have a lot of tissue damage and dead tissue. They need careful treatment to heal and avoid infections.
Surgical vs. Non-Surgical Debridement Methods
Debridement is vital for treating complex pressure wounds. It removes dead or infected tissue to help wounds heal. surgical debridement is best for quickly removing dead tissue from deep wounds. It’s very effective when fast action is needed.
non-surgical wound cleaning methods are better for some patients. They include enzymatic, autolytic, or biological options. These are good for patients who can’t have surgery or have wounds in hard-to-reach places.
The Significance of Removing Necrotic Tissue
Removing dead tissue is a big part of treating stage 4 pressure wounds. It lets doctors see the wound better and lowers the chance of infection. This makes healing faster and more effective.
| Method | Description | Indications | Benefits |
|---|---|---|---|
| Surgical Debridement | Physical removal of necrotic tissue using surgical instruments | Large amounts of devitalized tissue, urgency due to infection | Immediate results, complete removal of nonviable tissue |
| Enzymatic Debridement | Application of topical enzymatic agents to break down dead tissue | Smaller, non-infected wounds, or in combination with other methods | Specific targeting of necrotic tissue, can be used over longer periods |
| Autolytic Debridement | Utilizing the body’s enzymes and moisture to liquefy dead tissue | Patients with contraindications for surgical interventions | Minimal pain, preserves healthy tissue |
| Biological Debridement | Using sterile maggots to digest necrotic tissue | Non-healing wounds, unsuitable for surgical or sharp debridement | Natural, often effective in chronic wound conditions |
Advanced Therapies in the Treatment of Fourth Degree Pressure Ulcers
The field of wound care is always changing, with big steps forward in treating severe injuries like stage 4 pressure ulcers. Advanced therapies for pressure wounds and treatment innovations for stage 4 ulcers are key in managing these serious conditions well.
These new therapies aim to heal wounds faster and improve patients’ lives. They are making a big difference in treating fourth degree pressure ulcers.
- Oxygen Therapy: Boosts oxygen to wounds, helping them heal and grow back faster.
- Negative Pressure Wound Therapy (NPWT): Uses suction to help deep wounds heal better.
- Electrical Stimulation: Helps cells grow and wounds close with electrical impulses.
New treatment innovations for stage 4 ulcers also include biotechnology. This includes growth factor therapies and special topical solutions. They help wounds heal by activating and growing cells.
| Therapy | Description | Benefits |
|---|---|---|
| Oxygen Therapy | Delivers oxygen directly to the wound | Accelerates healing, reduces risk of infection |
| NPWT | Utilizes vacuum to promote healing | Decreases healing time, improves circulation |
| Electrical Stimulation | Applies electrical currents to the wound | Stimulates cell growth, enhances repair |
Adding these advanced therapies for pressure wounds to treatment plans is a big step forward. It offers hope for quicker and more effective healing. These new methods, though complex, are essential in treating severe wounds.
Regenerative Medicine: Hope for Severe Pressure Sore Healing
In the fast-changing world of wound care, regenerative medicine for wounds brings new hope. It uses advanced methods like stem cell therapy for ulcers and growth factors. These help wounds heal much faster.
Understanding Stem Cell Therapy in Wound Care
Stem cell therapy uses the body’s own repair tools. It’s a big step forward for treating long-lasting wounds, like severe pressure sores. This therapy helps fix damaged tissues, making it a key part of today’s wound care.
For those thinking about this therapy, it’s important to know about stem cell sources. The right stem cells are key to successful wound treatment.
Growth Factor Treatments and their Efficacy
Growth factors are another big part of regenerative medicine for wounds. Studies show they make wounds heal faster and better. These proteins help fix tissues, cutting down healing time and improving results.
To find out more about these treatments, check out this detailed guide.
With stem cell therapy for ulcers and growth factor treatments, there’s new hope for those with severe pressure sores. This modern method aims to not just heal wounds but also improve patients’ lives. It marks a new chapter in medical care.
Integration of Multidisciplinary Teams in Treatment Plans
Managing stage 4 pressure wounds needs more than just medical tools. It also requires a multidisciplinary treatment for pressure sores. This team-based approach brings together experts from different fields for interdisciplinary wound care. Their collaboration is key to addressing all a patient’s needs, improving outcomes.
Dealing with severe pressure sores is complex. Each team member’s skills and knowledge are combined. This creates a strong treatment plan that fits the patient’s health needs.
- Multidisciplinary teams include nurses, wound care specialists, dietitians, physiotherapists, and social workers.
- They also work with pharmacists for pain relief and infection prevention, a vital part of multidisciplinary treatment for pressure sores.
- Regular team meetings ensure everyone is in sync, which is essential for a successful treatment plan.
Now, let’s explore the roles each specialty plays in interdisciplinary wound care:
| Specialist | Role | Impact on Patient Outcomes |
|---|---|---|
| Nurses | Manage daily care, monitor healing | Direct influence on healing progress and patient comfort |
| Wound Care Specialists | Provide targeted therapies | Speeds up wound recovery with expert interventions |
| Dietitians | Assess nutritional needs and optimize diet for healing | Improves healing through nutritional support |
| Physiotherapists | Improve mobility | Reduces risk of further sores and enhances overall fitness |
| Social Workers | Support patient and family, manage care coordination | Helps align treatment with patient’s lifestyle and supports mental health |
In conclusion, using multidisciplinary treatment for pressure sores improves outcomes and healing. It also enhances the patient’s quality of life. This team approach in interdisciplinary wound care makes care holistic and tailored to each patient’s needs.
Developing a Personalized Care Plan
Personalized care is key for managing stage 4 pressure wounds. Tailoring treatment to each patient’s needs improves comfort and speeds up healing. This includes setting goals, involving caregivers, and adjusting the plan as needed.
Addressing Individual Patient Needs
Every patient faces unique challenges with severe pressure ulcers. Custom care plans consider the patient’s medical, dietary, and physical needs. These plans aim to heal wounds and reduce pain.
Setting Realistic Goals and Milestones
Setting clear goals is essential for recovery. Goals should be specific, measurable, achievable, relevant, and timely (SMART). Regular updates and adjustments keep the care plan in sync with the patient’s progress.
Family and Caregiver Involvement in Daily Wound Care
Family and caregivers play a big role in daily care. They need to know how to clean wounds, spot infections, and watch for changes. This education helps in providing better care and supports healing.
| Aspect of Care | Importance | Implementation Strategy |
|---|---|---|
| Regular Wound Assessment | Critical for early identification of complications | Training caregivers in recognizing and reporting changes in wound condition |
| Emotional and Psychological Support | Essential for patient’s mental health and stress reduction | Including family members in treatment discussions to support patient’s well-being |
| Nutritional Guidance | Paramount to support wound healing and overall health | Providing tailored diet plans and education on nutrient-rich foods beneficial for skin integrity |
Monitoring and Adjusting Treatment for a Stage 4 Pressure Wound
Managing stage 4 pressure wounds well needs careful treatment monitoring for pressure wounds and adjusting care for stage 4 ulcers. This approach makes sure treatments fit the patient’s changing needs. It helps in healing faster and lowers the risk of problems.
Keeping a close eye on the patient’s progress is key. This means checking how well the treatment is working and making changes when needed. This flexible care is very important for patients with complex needs. Their wounds can change quickly.
- Regular checks to see how the wound is healing and if there are any signs of infection or getting worse.
- Changing the wound care plan based on what these checks show.
- Working with a team of different healthcare professionals for a complete treatment plan.
Changing treatment plans might mean changing medicines, using new wound care tools, or adjusting what the patient eats. These changes are important for helping stage 4 ulcers heal better.
In short, keeping a close watch and being ready to change treatment plans is key to managing severe pressure wounds. By focusing on making care fit each patient and keeping a close eye on them, doctors can greatly improve how well stage 4 ulcers are treated.
Preventing Recurrence: Strategies for Long-Term Care
Healing a stage 4 pressure wound is a big win in patient care. But, the fight doesn’t stop there. Preventing pressure sore recurrence is key to keeping those most vulnerable healthy. Long-term care strategies help keep the victory over past wounds alive.
Regular skin checks are the first line of defense against pressure sores coming back. Watching for signs like redness and warmth helps catch problems early. This way, we can stop them before they get worse.
Managing risks is another important part of preventing recurrence. This includes moving patients often, taking good care of their skin, and using the right support surfaces. It’s also about keeping them hydrated and well-nourished. Making lifestyle changes, like moving more and learning about avoiding pressure, helps too. Tools like pressure-relieving cushions and mattresses also play a big role in reducing the risk of wounds coming back.
In short, creating a strong system that focuses on skin health, education, and action is essential. By doing regular skin checks, managing risks, and making lifestyle changes, we can keep stage 4 pressure wounds from coming back. Our goal is to heal and then keep that healing going, improving the patient’s life quality in the long run.
FAQ
Q: What is a Stage 4 Pressure Ulcer?
A: A Stage 4 pressure ulcer is a serious condition. It involves full-thickness skin and tissue loss. This can expose bone, tendon, or muscle. These wounds are at high risk for infection and need complex care.
Q: Why is a deep tissue injury considered severe?
A: Deep tissue injuries are severe because they affect deeper tissue layers. They may not be visible right away. This makes early detection and treatment hard.
Q: How can I recognize the signs and symptoms of a Stage 4 Pressure Ulcer?
A: Signs include exposed bone, muscle, or tendons, and large skin loss. You might also see tunneling and significant pain. Look for signs of infection like pus, odor, heat, and redness.
Q: What are the main causes and risk factors for developing a Stage 4 Pressure Ulcer?
A: Main causes are sustained pressure, shear, and friction. Risk factors include immobility, nutritional deficiencies, age, incontinence, and conditions that affect blood flow.
Q: How is a Stage 4 Pressure Wound accurately diagnosed?
A: Diagnosis involves a healthcare professional’s thorough assessment. They use visual examination and imaging tests. They also look at the patient’s medical history and risk factors.
Q: What are some proper wound cleaning protocols for a Stage 4 Pressure Ulcer?
A: Protocols include gentle irrigation to remove debris. They use non-cytotoxic antiseptics to reduce infection. Careful debridement removes non-viable tissues.
Q: How are infections in Stage 4 Pressure Ulcers prevented and controlled?
A: Infection prevention involves meticulous wound cleaning and dressing changes. Appropriate antibiotics are used. Monitoring for systemic infection signs is also key.
Q: What role does nutrition play in the healing of a Stage 4 Pressure Wound?
A: Nutrition is vital for wound healing. It provides the nutrients needed for tissue repair. A well-balanced diet with protein, vitamins, and minerals is essential.
Q: What pain management strategies are available for patients with Stage 4 Bed Sores?
A: Pain management includes pharmacological treatments like analgesics. Non-pharmacological approaches include pressure relief and proper wound care. Psychological support is also important.
Q: What are the debridement options for Stage 4 Pressure Wounds?
A: Debridement options include surgical removal of necrotic tissue. Non-surgical methods like enzymatic, autolytic, or biological debridement are also used. The choice depends on the individual’s condition and wound characteristics.
Q: Can advanced therapies and regenerative medicine play a part in treating Stage 4 Pressure Ulcers?
A: Yes, treatments like stem cell therapy and growth factor treatments are advances in wound care. They can stimulate tissue repair and promote healing of severe pressure ulcers.
Q: Why is a multidisciplinary team important in the treatment of Stage 4 Pressure Ulcers?
A: A multidisciplinary team provides complete care. They combine various expertise to address all aspects of wound care and patient needs effectively.
Q: How does caregiver involvement contribute to the management of Stage 4 Pressure Ulcers?
A: Caregiver involvement is key for daily wound management. They provide emotional support, assist with mobility, and ensure treatment adherence outside the clinic.
Q: Why is it important to monitor and adjust treatment for a Stage 4 Pressure Wound?
A: Continuous monitoring and treatment adjustments are vital. They help respond to changing wound conditions, promote healing, and prevent complications.
Q: What strategies can help prevent the recurrence of Stage 4 Pressure Wounds?
A: Prevention strategies include regular skin assessments and maintaining nutrition. Managing moisture and pressure on vulnerable areas is also important. Educating patients and caregivers on skin care and risk management helps.
Go to the full page to view and submit the form.