Type 1 diabetes is a complex condition with many causes. Understanding the causes of diabetes mellitus type 1 is key. It involves genetic, autoimmune, and environmental factors.
These risk factors work together to increase the chance of getting the disease. We aim to explain how these factors can lead to type 1 diabetes.
Knowing these causes is important. It helps us find ways to prevent and treat the disease. This introduction is the first step in understanding and fighting type 1 diabetes.
Understanding Type 1 Diabetes
Type 1 diabetes is a chronic condition where the body’s autoimmune response attacks and destroys insulin-producing cells in the pancreas. These cells, known as pancreatic beta cells, are key for making insulin. Insulin helps control blood sugar levels. When these cells are damaged, the body can’t make enough insulin, leading to high blood sugar.
The body’s immune system mistakenly attacks its own insulin-producing cells. This attack reduces the number of working pancreatic beta cells. With fewer cells, the body can’t make enough insulin, causing blood sugar to rise.
To better understand, here’s a detailed look at how beta cell destruction and insulin deficiency occur:
| Stage | Description | Impact on Insulin Production |
|---|---|---|
| Initial Autoimmune Activation | Immune system starts to target pancreatic beta cells. | Little change in insulin production, often not noticed. |
| Progressive Beta Cell Destruction | Continued attack reduces insulin-producing cells. | Noticeable changes in blood sugar; insulin therapy might be needed. |
| Advanced Insulin Deficiency | Most pancreatic beta cells are destroyed. | Long-term high blood sugar; full insulin replacement therapy is required. |
Understanding how the immune system and pancreatic beta cells interact shows the importance of the autoimmune response in type 1 diabetes. This knowledge helps in diagnosing and managing the condition. It also guides in finding ways to keep the body’s insulin-making ability as strong as possible.
Hereditary Disposition and Genetic Factors
Looking into Type 1 diabetes shows a mix of genetic factors that make some people more likely to get it. A big part of this is family history. If your family has Type 1 diabetes, you’re more at risk.
Genetic research has found certain genetic markers linked to Type 1 diabetes. This helps us understand it better and find ways to manage it early on.
The Role of Family History in Type 1 Diabetes
If your family has Type 1 diabetes, you’re more likely to get it. Research shows that having a first-degree relative with Type 1 diabetes raises your risk to 15%. This is much higher than the 0.4% risk for everyone else.
Identifying Genetic Markers for Type 1 Diabetes
Scientists are working hard to find specific genetic markers for Type 1 diabetes. Finding these markers early can help doctors create better treatment plans. It also helps identify who might be at risk.
A major study found several genes linked to a higher risk of Type 1 diabetes. The Human Leukocyte Antigen (HLA) complex was the most important. By studying how these genes work with the environment, scientists aim to understand Type 1 diabetes better.
To learn more about how genetics play a role in diseases, check out how Alzheimer’s Disease is linked to genetics. It’s similar to how genetics affect Type 1 diabetes in families.
Autoimmune Response Leading to Type 1 Diabetes
Type 1 Diabetes is caused by an autoimmune response. The immune system, which fights infections, attacks the body’s islet cells in the pancreas. This leads to a chronic condition known as Type 1 Diabetes.
What Triggers the Autoimmune Attack?
Finding out what starts the autoimmune attack is key. Triggers include genetics, environment, and viruses. But what exactly sets off the immune system to attack the body’s insulin-making cells is a mystery scientists are trying to solve.
The Development of Islet Cell Antibodies
In people at risk for Type 1 Diabetes, islet cell antibodies are early signs. These antibodies show the immune system is starting to attack the wrong cells. The cells that make insulin are being destroyed.
Islet cell antibodies are found before Type 1 Diabetes symptoms show up. Knowing about them helps predict the disease. It also helps in finding ways to stop or slow down diabetes.
Causes of Diabetes Mellitus Type 1
The causes of diabetes mellitus type 1 involve genetics, the immune system, and the environment. This autoimmune disease destroys insulin-producing cells in the pancreas. The immune system mistakenly attacks these cells.
Genetics are a key factor in developing type 1 diabetes. But, not everyone with these genes will get the disease. Environmental factors also play a role in starting the autoimmune attack.
- Immune system dysfunction is at the core of this condition, where an erroneous attack is launched against the body’s own cells.
- Significant environmental contributors include viral infections, dietary factors, and possibly even early exposure to certain allergens.
- Continuing immune system stimulation may lead to the progressive destruction of the beta cells in the pancreas.
The loss of these cells stops insulin production. Insulin is key for controlling blood sugar levels. Without it, blood sugar levels stay high, a hallmark of type 1 diabetes.
| Factor | Role in Type 1 Diabetes |
|---|---|
| Genetic Susceptibility | Provides the framework upon which environmental factors can act. |
| Autoimmune Reaction | Primary mechanism destroying insulin-producing cells. |
| Environmental Triggers | Activates immune system leading to diabetes onset. |
Research on causes of diabetes mellitus type 1 is ongoing. Scientists are learning more about how the immune system mistakenly attacks insulin-producing cells. This knowledge may help find ways to prevent the disease in the future.
The Link Between Viral Infections and Type 1 Diabetes
Research is looking into how viral infections might start Type 1 diabetes. They focus on how these infections can trigger the body’s immune system to attack itself. This idea, known as the diabetes viral links hypothesis, explores if certain viruses can cause the immune system to destroy insulin-making cells in the pancreas.
Common Viruses Implicated in Type 1 Diabetes
Several common viruses have been linked to Type 1 diabetes. These include Enterovirus, like Coxsackie B virus, mumps virus, and rubella virus. Research shows that these viral infections might start the autoimmune process that leads to the disease.
Understanding the Viral Trigger Theory
The viral trigger theory suggests that these viruses can directly harm pancreatic beta cells or cause inflammation. This inflammation can indirectly destroy cells. Studies have found viral RNA in the pancreas of people with new Type 1 diabetes. This theory is changing how we think about and treat diabetes viral links.
Environmental Triggers for Type 1 Diabetes
This section looks into how our surroundings can affect our health. It explores how diet, lifestyle, and early life exposures might raise the risk of Type 1 diabetes.
How Diet and Lifestyle May Influence Diabetes Risk
Recent studies show that dietary factors play a big role in lifestyle diabetes risk. Diets full of processed sugars and fats can lead to autoimmune reactions, which are key in Type 1 diabetes. On the other hand, eating more fiber, whole grains, and omega-3 fatty acids might help protect against it.
- High-sugar diets may increase body inflammation, a precursor to autoimmune responses.
- Foods rich in omega-3 fatty acids, such as fish and flax seeds, might reduce inflammation.
Our dietary choices have a big impact, made even bigger by our lifestyle habits. These include how much we exercise, how we handle stress, and our exposure to toxins. All these factors greatly affect our overall health and diabetes risk.
The Impact of Early Life Exposures
Exposures in early life can shape our health for the rest of our lives. Factors like pollutant exposure, what our mothers eat during pregnancy, and how we’re fed as babies are very important. For example, introducing cow’s milk and gluten early on might increase the risk of Type 1 diabetes.
Other lifestyle factors, like how active we are and where we live, also play a role. These can affect when diabetes starts through different but connected ways.
To lower Type 1 diabetes risk, we need to tackle these issues from all sides. Encouraging healthier eating habits from the start and making better lifestyle choices can help reduce diabetes’s impact.
Destruction of Insulin-Producing Cells
Type 1 diabetes is caused by the immune system attacking the insulin-producing cells in the pancreas. This attack is key to the disease, causing a lack of insulin. Without enough insulin, the body can’t control blood sugar levels.
The immune system’s attack on pancreatic beta cells happens slowly over time. It’s important to understand this to find ways to protect these cells. This could help prevent type 1 diabetes.
- Initial immune system misidentification of beta cells as foreign
- Progressive inflammatory response leading to cell destruction
- Subsequent insulin-producing cell failure
- Final onset of symptomatic diabetes following significant beta cell loss
Studying how to stop this autoimmune destruction is promising. It could help predict and maybe even reverse type 1 diabetes.
| Stage of Destruction | Impact on Insulin Production | Percentage of Beta Cells Affected |
|---|---|---|
| Initial Recognition | Minor Decrease | 20% |
| Active Autoimmunity | Moderate Decrease | 50% |
| Extensive Damage | Significant Loss | 80% or more |
Keeping pancreatic beta cells safe and acting early is what researchers are focusing on. They aim to stop the autoimmune destruction before it’s too late. Early diagnosis and quick action are key.
Immune System Malfunction and Its Consequences
The immune system malfunction in type 1 diabetes is complex. It mainly causes beta cell destruction. This is a key event that leads to serious type 1 diabetes consequences. This issue affects glucose regulation and causes many other problems.
An autoimmune attack is at the heart of this issue. It mistakenly attacks and destroys insulin-making beta cells in the pancreas. This makes it hard for the body to keep blood sugar levels balanced. People with type 1 diabetes must take insulin for life.
The long-term effects of beta cell destruction and unstable insulin levels are severe. They can cause vision loss, kidney failure, and heart disease. It’s important to understand how immune system malfunction leads to these problems. This knowledge helps in finding better treatments. For more on this, check out the new treatments discussed here.
| Consequence | Description | Impact on Life Quality |
|---|---|---|
| Vision Impairment | High blood sugar levels damage the tiny blood vessels in the retina, leading to diabetic retinopathy. | Can lead to blindness if not managed properly. |
| Kidney Failure | The kidneys’ filtering system is damaged, which may require dialysis or a kidney transplant. | Significantly alters daily activities and health. |
| Cardiovascular Disease | Increased risk of heart attacks, strokes due to damaged blood vessels and nerves. | May result in early mortality and reduced physical capability. |
It’s key to tackle the root causes of immune system malfunction. More research into treatments like CAR T-cell therapy could lead to new ways to fight beta cell destruction and type 1 diabetes consequences.
Childhood Risk Factors for Type 1 Diabetes
It’s key to know the risks for childhood diabetes to act early. This part talks about how age and early signs are vital for spotting and handling type 1 diabetes in kids.
The Role of Age in Developing Type 1 Diabetes
Age is a big deal in getting type 1 diabetes. It can happen at any age, but mostly in kids and teens. The risk goes up when they start puberty, due to the big hormonal changes.
This shows why it’s so important to watch for diabetes signs, mainly during this key growth time.
Early Detection Signs in Children
Spotting early signs of childhood diabetes is key to quick treatment and avoiding big problems. Look out for signs like drinking a lot of water, going to the bathroom a lot, losing weight without trying, and feeling really tired. These are often seen as normal kid stuff, but they’re not.
Parents and caregivers need to keep an eye out, even more so if diabetes runs in the family.
Here are some important tips for spotting early signs:
- Watch for changes in behavior like being really cranky or super tired.
- See if your child is eating more or less than usual.
- Look for signs of dehydration, as it can mean high blood sugar.
Acting fast is very important. Keeping blood sugar levels in check can stop or slow down diabetes problems. If you see any of these signs, get your child checked by a doctor right away.
Knowing these risks and signs can help catch diabetes early. This can make managing it easier for your child’s whole life.
Various Stages of Pancreatic Beta Cell Destruction
Understanding Type 1 diabetes involves knowing the stages of beta cell destruction. These stages are key in the transition from health to disease. The immune system’s attack on beta cells is not sudden but goes through clear stages. These stages lead to the onset of diabetes.
Initial Beta Cell Targeting by the Immune System
The first stage of Type 1 diabetes is when the immune system attacks beta cells. This autoimmune response is the main cause of diabetes. The body sees these insulin-making cells as threats.
The destruction starts quietly and is often missed until many cells are harmed.
The Progression to Overt Diabetes
The attack on beta cells gets worse, leading to less insulin production. This phase moves from trying to keep up, to failing to control blood sugar. It’s a key point where diabetes symptoms show up, needing medical help.
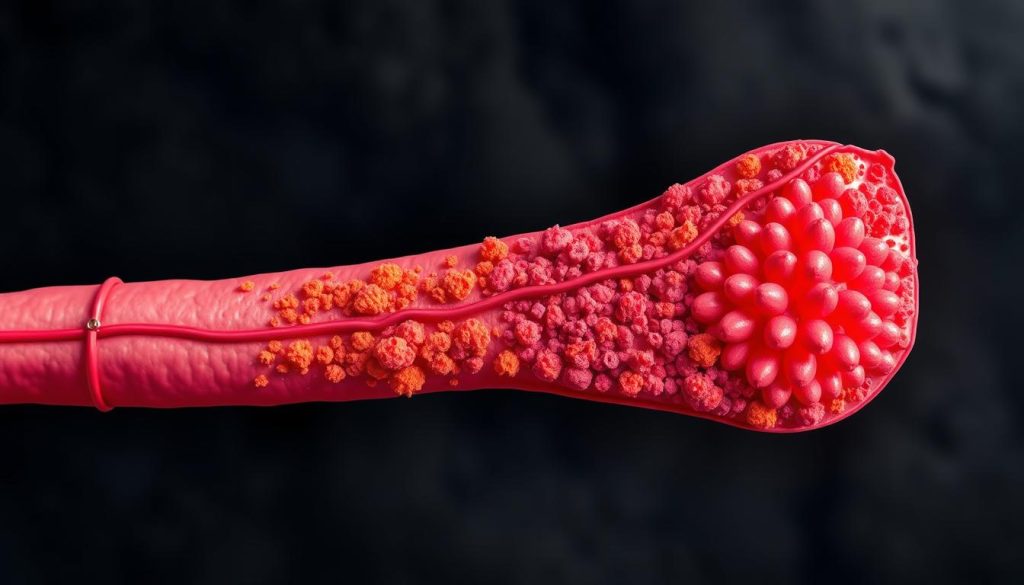
Watching and understanding these changes is key for early Type 1 diabetes treatment. It could help delay or stop the disease. The stages of beta cell destruction show the need for more research and new treatments to fight diabetes.
Hormonal Changes as a Risk Factor
Looking into how hormonal changes affect diabetes risk is key, mainly during big life changes. Hormonal shifts can trigger endocrine factors that might make people more likely to get type 1 diabetes. For example, the rise of hormones like estrogen and testosterone in puberty can change how well insulin works. This could raise the chance of getting type 1 diabetes.
It’s important to see how hormonal changes and diabetes risk are linked. The endocrine system is key in keeping hormone levels right, which affects how we metabolize food. When this balance gets upset, it can affect diabetes risk and how well our immune system works.
- Increased hormone levels during puberty
- Fluctuations in hormonal balance during pregnancy
- Changes in stress hormones and their impact on glucose levels
These times are key for looking at how endocrine factors play a part in diabetes. Below is a look at how hormones change at different times in life and how they affect diabetes risk.
| Life Stage | Key Hormonal Changes | Impact on Diabetes Risk |
|---|---|---|
| Puberty | Increases in estrogen and testosterone | Higher insulin resistance |
| Pregnancy | Higher levels of placental hormones | Temporary insulin resistance |
| Menopause | Decline in estrogen and progesterone | Varies, possible increase in type 2 diabetes risk |
It’s clear we need to watch hormonal changes closely to prevent diabetes. Seeing these changes as important endocrine factors could help us find better treatments for each person’s life stage and hormone levels.
Influence of Dietary Factors on Type 1 Diabetes
Looking into how different foods might affect type 1 diabetes is key. It helps us understand this autoimmune disease better. Some foods might trigger or prevent it.
Does Cow’s Milk Trigger Type 1 Diabetes?
The link between cow’s milk and type 1 diabetes is a big debate. Some research says cow’s milk proteins could start an immune reaction. This could lead to type 1 diabetes in some people.
Some studies point to bovine serum albumin in cow’s milk. They think it might cause autoimmune attacks on the pancreas.
The Role of Nutritional Toxins
Nutritional toxins are a big worry in the fight against type 1 diabetes. These toxins can be found in foods or added during farming. They might harm the pancreas or mess with the immune system.
The connection between diet and immune response is complex. Some toxins in food might make autoimmune diseases worse or start them.
- Studies on cow’s milk proteins and their effects on children at risk.
- Research on how toxins in food and the environment affect type 1 diabetes.
Psychological Stress and Type 1 Diabetes
The link between psychological stress and type 1 diabetes development is being studied more. It looks at how long-term emotional stress can harm the immune system and insulin-making cells. Knowing how stress works in the body is key to finding ways to stop or slow down type 1 diabetes.
Exploring the Stress-Diabetes Link: It’s thought that ongoing stress can start a chain of reactions in the body. These reactions might lead to type 1 diabetes. Stress could also make the body attack its own pancreatic cells, a big part of type 1 diabetes development.
- Immune System Disruption: Long-term stress can mess with how the immune system works. This might raise the chance of getting autoimmune diseases like type 1 diabetes.
- Cortisol Overproduction: Stress over time can cause too much cortisol. This can mess with insulin making and how the body handles sugar.
- Beta Cell Function: Stress hormones can hurt the health of beta cells. This makes it harder for them to make enough insulin.
| Stress Factor | Impact on Diabetes Risk | Area of Effect |
|---|---|---|
| Chronic Psychological Stress | Potential to trigger autoimmune response | Immune System |
| Elevated Cortisol Levels | Impairs insulin regulation and glucose management | Endocrine System |
| Stress-induced Inflammation | May lead to beta cell damage | Pancreatic Health |
Understanding the stress response in the body is complex. More research is needed to really grasp its role in type 1 diabetes development. Ways to reduce stress could be part of a bigger plan to stop or slow down type 1 diabetes, mainly for those at high risk.
The Role of Physical Activity in Diabetes Prevention
Regular physical activity is key to preventing many health problems, including type 1 diabetes. It helps control the immune system, playing a big role in diabetes prevention and overall health.
Exercise as an Immune Modulator
Exercise immune modulation means how physical activity changes the immune system. It makes the immune system work better and reduces inflammation. This can lower the risk of diseases like type 1 diabetes.
Studies show that regular, moderate exercise can change the immune system. It helps prevent autoimmune reactions that can damage pancreatic beta cells.
Physical Activity Guidelines for At-Risk Individuals
People at risk of type 1 diabetes should follow specific physical activity guidelines. They should do at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise each week. They should also do muscle-strengthening activities on two or more days a week.
These activities help prevent diabetes and improve immune function. They also lead to better overall health.
| Type of Activity | Duration | Frequency |
|---|---|---|
| Moderate Aerobic Activity | 150 minutes | Weekly |
| Vigorous Aerobic Activity | 75 minutes | Weekly |
| Muscle-Strengthening | Varying | 2 days per week |
Screening and Preventive Strategies
In the fight against type 1 diabetes, diabetes screening and preventive strategies are key. They help protect at-risk populations. Early detection and care can change the disease’s course, maybe even prevent it.
Good diabetes screening programs find early signs of glucose problems. This is very important for those with a family history of diabetes or other risk factors. New biomarkers and better diagnostic tools have made these screenings more accurate.
- Genetic testing for newborns and young kids to find those at risk.
- Annual blood sugar tests for teens and adults at risk.
- Watching blood sugar closely for those who had gestational diabetes.
Along with screening, there are preventive strategies. These include lifestyle changes to lower diabetes risk, mainly for those at risk. Teaching about diet and exercise is key.
| Preventive Measure | Description | Target Group |
|---|---|---|
| Nutritional Education | Programs on how carbs and sugars affect blood sugar. | All at-risk populations |
| Physical Activity Encouragement | Getting people to exercise more every day. | Youth and adults with obesity |
| Regular Medical Check-ups | Regular health checks to adjust prevention plans. | People with a family history of diabetes |
By using a mix of diabetes screening and preventive strategies, doctors can lower type 1 diabetes risk in at-risk populations. The way to prevent it is complex but starts with early detection and ongoing care.
Innovative Research and Emerging Theories
Scientists are working hard to find a cure for Type 1 diabetes. They are studying the disease in new ways. This includes looking at how the immune system attacks the pancreas, which is key to making insulin.
Gene editing is also being explored. It could fix or replace genes that don’t work right. This might lead to a permanent cure for Type 1 diabetes.
Researchers are also looking at how our gut bacteria affect diabetes. They think that changing our gut bacteria could help prevent Type 1 diabetes. This is a new way of thinking about treating diabetes, combining science and nutrition.
Another area of research is immunomodulation therapies. These are drugs that can control the immune system. They might help manage Type 1 diabetes without the need for insulin shots.
As we move forward, researchers are filled with hope. They are working hard to find new ways to treat Type 1 diabetes. Their efforts give hope to millions of people around the world.
FAQ
Q: What are the risk factors for developing Type 1 Diabetes?
A: Risk factors include autoimmune responses and genetic factors. Environmental influences also play a role. A family history of diabetes can increase your risk.
Q: How does Type 1 Diabetes occur in the body?
A: Type 1 Diabetes happens when the immune system attacks insulin-producing cells. This results in a lack of insulin and high blood sugar.
Q: Can genetic markers predict Type 1 Diabetes?
A: Researchers are looking for genetic markers to predict Type 1 Diabetes. But, more research is needed for accurate predictions.
Q: What triggers the autoimmune attack in Type 1 Diabetes?
A: The exact triggers for the autoimmune attack are not known. It might involve environmental factors, viruses, or other unknown factors.
Q: What are islet cell antibodies, and what role do they play in Type 1 Diabetes?
A: Islet cell antibodies are proteins that target and damage insulin-producing cells. This leads to Type 1 Diabetes.
Q: Are viral infections linked to Type 1 Diabetes?
A: Some studies suggest viral infections might trigger Type 1 Diabetes. But, more research is needed to confirm this.
Q: How might diet and lifestyle influence the risk of developing Type 1 Diabetes?
A: Diet and lifestyle might affect your risk of Type 1 Diabetes. Early dietary exposures or lack of physical activity could play a role. But, the connections are complex and not fully understood.
Q: What happens when insulin-producing cells are destroyed?
A: When insulin-producing cells are destroyed, insulin levels drop. This is essential for regulating blood sugar. It leads to high blood sugar levels in Type 1 Diabetes.
Q: What are the consequences of immune system malfunction in Type 1 Diabetes?
A: A malfunctioning immune system can destroy pancreatic beta cells. This results in insulin deficiency. It can lead to severe complications due to uncontrolled blood sugar levels.
Q: What are the childhood risk factors for Type 1 Diabetes?
A: Childhood risk factors include genetic predisposition and environmental exposures. The presence of certain antibodies and infections during infancy or early childhood might also play a role.
Q: At what stages do pancreatic beta cells get destroyed in Type 1 Diabetes?
A: Pancreatic beta cells are targeted by the immune system early on. Their destruction leads to prediabetes and eventually Type 1 Diabetes as pancreatic function declines.
Q: How do hormonal changes influence the risk of Type 1 Diabetes?
A: Hormonal changes, like those during puberty, can affect the immune system and insulin needs. This might influence the risk of Type 1 Diabetes.
Q: Does cow’s milk trigger Type 1 Diabetes?
A: The idea that cow’s milk triggers Type 1 Diabetes is debated. Some studies suggest a link, but more research is needed to confirm it.
Q: What is the relationship between psychological stress and Type 1 Diabetes?
A: Chronic stress might affect the immune system and beta cell function. But, the direct link between stress and Type 1 Diabetes is not fully understood.
Q: Can physical activity prevent Type 1 Diabetes?
A: Physical activity may have benefits for the immune system and overall health. It could potentially lower the risk of Type 1 Diabetes. But, it’s not a guarantee for prevention.
Q: How can Type 1 Diabetes be screened and prevented?
A: Type 1 Diabetes can be screened through blood glucose monitoring and autoantibody tests. Preventive strategies are being researched. Some focus on modulating the immune system response in at-risk individuals.
Q: What new research is emerging in the field of Type 1 Diabetes?
A: New research includes studies on immunotherapy and beta cell regeneration. It also involves genetic risk profiling and novel insulin delivery systems. These aim to improve management and patient outcomes.
Go to the full page to view and submit the form.