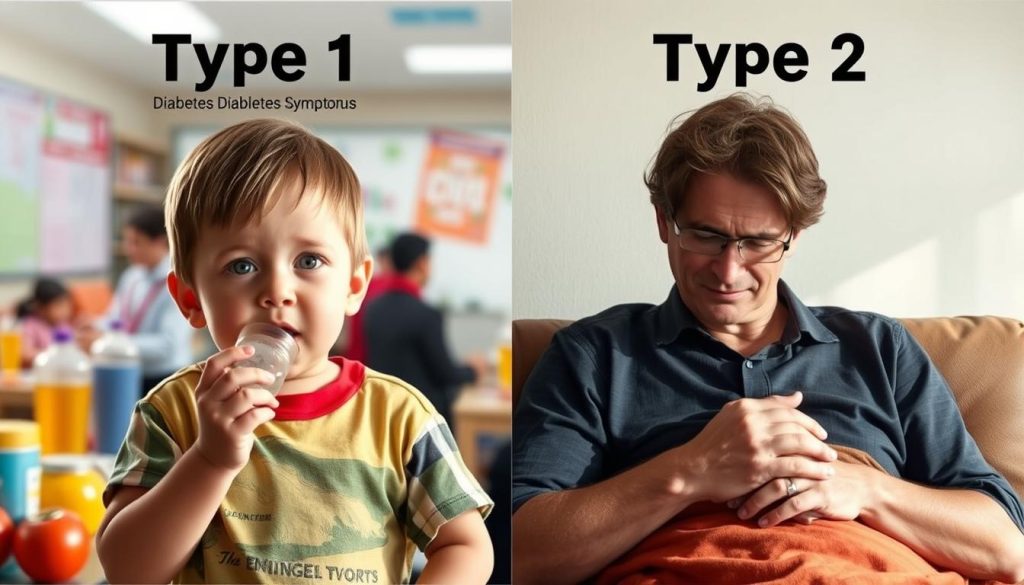
The type 1 and type 2 diabetes mellitus difference is more than just numbers. It shows different causes, ways to manage, and challenges for those affected. Understanding these differences is key to better care and grasping the global health issue.
The Centers for Disease Control and Prevention (CDC) highlights the differences between the two diseases. They focus on causes, symptoms, and how to treat them. Knowing about understanding diabetes types is essential.
The American Diabetes Association (ADA) is working hard to raise awareness about diabetes. This effort is important for managing the disease. The World Health Organization (WHO) also plays a role by creating plans to tackle these diseases in a specific way. This helps us understand the diabetes differences breakdown better.
Understanding Diabetes Mellitus and Its Types
Diabetes mellitus is a group of metabolic disorders. They all have high blood sugar levels. The pancreas’s beta cells, which make insulin, are damaged or gone. This leads to type 1 or type 2 diabetes.
It’s key to know the diabetes mellitus variances. This is because the NIDDK and Mayo Clinic say so. They give us the details we need.
Managing diabetes means understanding its types. This is why diabetes mellitus comparison is so important. The IDF says we need to diagnose and treat each type right.
| Type of Diabetes | Pathophysiology | Usual Onset | Common Treatments |
|---|---|---|---|
| Type 1 Diabetes | Autoimmune destruction of insulin-producing beta cells | Childhood or Adolescence | Insulin injections, carbohydrate counting |
| Type 2 Diabetes | Insulin resistance and eventual impairment in insulin secretion | Adult, mostly after 45 years | Diet modifications, oral medications, sometimes insulin |
Knowing the differences is vital. It helps doctors, teaches patients, and fights diabetes worldwide. The diabetes mellitus variances help us treat and prevent diabetes better.
Defining Type 1 Diabetes: An Autoimmune Disorder
Type 1 diabetes is different from type 2 in key ways. It’s an autoimmune disorder where the immune system attacks the body’s cells. This condition destroys beta cells in the pancreas, which make insulin.
Overview of Type 1 Diabetes Pathophysiology
Type 1 diabetes comes from a mix of genetics and immune system problems. The immune system attacks the pancreas’s beta cells. This leads to a lack of insulin, which is key for blood sugar control.
This is a big difference from type 2 diabetes, which is more about insulin resistance. Organizations like JDRF are working hard to find ways to stop or fix this damage.
The Role of Genetics and Environmental Factors in Type 1 Diabetes
Genetics are important in type 1 diabetes, but the environment can trigger it. Studies show viruses and other factors can start the autoimmune attack. This makes managing and preventing type 1 diabetes more complex.
Research from the National Institute of Environmental Health Sciences (NIEHS) shows type 1 diabetes is caused by many factors. Finding genetic markers early and watching for environmental risks could help prevent it.
Dealing with type 1 diabetes affects more than just health. Understanding the link between diabetes and hair loss helps manage side effects. Knowing the difference between type 1 diabetes vs type 2 diabetes is key for better treatments and education.
Exploring Type 2 Diabetes: A Lifestyle-Related Condition
Type 2 diabetes is a big deal in the world of non-communicable diseases. It’s closely linked to how we live, like what we eat and how much we move. The American Heart Association, the CDC, and Merck Manuals give us a lot of information on how diet and exercise affect diabetes.
Distinguishing Type 2 Diabetes by Insulin Resistance
Insulin resistance is key in type 2 diabetes. It means our cells don’t use insulin well. This leads to high blood sugar, which can cause big health problems if not handled right. Seeing how insulin sensitivity differs in people with and without type 2 diabetes shows how important it is to keep an eye on insulin levels.
Lifestyle Elements: Diet and Exercise Influence
Changing how we live is a big part of managing type 2 diabetes, says the CDC. Eating right and staying active can really help. Studies show that being overweight, eating badly, and not moving enough can make diabetes worse.
| Factor | Impact on Type 2 Diabetes | Recommended Action |
|---|---|---|
| Diet | High sugar and fat intake increases risk | Adopt a balanced diet rich in nutrients |
| Exercise | Lack of physical activity enhances insulin resistance | Incorporate regular exercise regimes |
| Obesity | Major risk factor for developing type 2 diabetes | Maintain healthy body weight |
Getting to know diabetes types and how they relate to our lifestyle is key to managing and preventing them. For type 2 diabetes, knowing about insulin resistance and how lifestyle changes can help shows the importance of taking care of our health.
Differences in Age of Onset: Pediatric vs Adult Diagnosis
The age when people get type 1 and type 2 diabetes is a key difference. Type 1 diabetes often starts in kids and teens, known as juvenile diabetes. Type 2 diabetes, linked to lifestyle, used to start in adults. But now, we see more cases in younger people, making the type 1 and type 2 diabetes mellitus difference more important.
A study by the Pediatric Endocrine Society shows a worrying trend. Type 2 diabetes is becoming more common in kids. This is due to more obesity, less exercise, and unhealthy diets in young people.
| Diabetes Type | Typical Age of Onset | Recent Trends |
|---|---|---|
| Type 1 Diabetes | Childhood to Adolescence | Stable incidence but improved diagnostic methods |
| Type 2 Diabetes | Adults (Over 40 years) | Increasingly appearing in younger age groups |
This change affects not just health but society too. Early type 2 diabetes can lead to more health problems. So, we need better screening and prevention for young people.
Knowing when each type of diabetes starts helps us treat it better. It leads to more research and better care for people of all ages. This could improve health outcomes for everyone.
Type 1 and Type 2 Diabetes Mellitus Difference in Symptoms
It’s key to know the differences in symptoms between type 1 and type 2 diabetes mellitus. This knowledge helps in understanding diabetes types and how to manage them. Both types have some similar symptoms, but how they start and how bad they are can differ a lot. This shows why it’s important to spot these differences.
Identifying Common Symptoms in Both Diabetes Types
Type 1 and type 2 diabetes share some symptoms that are important for diagnosis. These include feeling very thirsty, needing to pee a lot, and feeling tired. These signs are key to getting medical help and are often the first signs of the disease.
Differences in Symptom Severity and Onset
The way symptoms start and how bad they are can tell us about the diabetes type. Symptoms of type 1 diabetes come on fast and can be very severe. This can lead to health problems quickly if not treated right away.
On the other hand, symptoms of type 2 diabetes start slowly and may take years to show up. This slow start can make it harder to catch the disease early. It also means there’s a higher chance of serious problems later on.
| Symptom | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Onset | Rapid | Gradual |
| Severity | More intense | Less intense initially |
| Common Symptoms | Frequent urination, extreme hunger, unintended weight loss | Frequent urination, increased thirst, blurred vision |
This comparison helps us understand diabetes types better. It also shows why we need different ways to treat these diabetes mellitus variances effectively.
Investigating Insulin Dependency in Diabetes Types
In understanding the type 1 and type 2 diabetes mellitus difference and diabetes types contrast, one key aspect is insulin’s role. Both types of diabetes affect blood glucose management. Yet, insulin use differs, showing their unique disruptions.
The Necessity of Insulin in Type 1 Diabetes Management
Type 1 diabetes often hits children and young adults. It’s when the pancreas can’t make insulin because of an autoimmune attack. The Juvenile Diabetes Research Foundation (JDRF) says people with type 1 diabetes need insulin forever.
This is because their body can’t make insulin. So, they must get insulin from outside to keep blood sugar in check and avoid serious problems.
Type 2 Diabetes: Insulin and Alternative Treatments
Type 2 diabetes usually starts in adults and is linked to lifestyle and genes. The American Diabetes Association (ADA) says insulin might be needed for type 2 diabetes if diet and pills don’t work. The ADA also talks about other treatments like pills, GLP-1 receptor agonists, and lifestyle changes.
| Treatment | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Insulin | Required | Often later in disease progression |
| Oral Hypoglycemics | Not applicable | Commonly used |
| Lifestyle Changes | Supportive role | Can be primary treatment |
| GLP-1 Receptor Agonists | Not typical | Increasingly utilized |
Knowing how insulin and other treatments differ for type 1 and type 2 diabetes is key. It helps in making treatment plans that fit each person. It also shows how complex diabetes is as a health issue.
Diabetes Mellitus Comparison: Risk Factors and Prevention
Understanding the understanding diabetes types is key. Knowing the risk factors and prevention strategies is essential. The National Institutes of Health (NIH), Centers for Disease Control and Prevention (CDC), and Harvard School of Public Health offer valuable insights. These insights help shape public health policies and individual prevention plans.
It’s important to know how risk factors differ between Type 1 and Type 2 diabetes. Type 1 diabetes is often linked to genetics and autoimmune issues, with no known prevention. On the other hand, Type 2 diabetes is influenced by lifestyle and weight, where prevention is possible.
- Familial history is a major risk factor for both types, the NIH says.
- Poor diet and lack of exercise are big risks for Type 2 diabetes, the CDC notes.
- Viruses may trigger Type 1 diabetes, NIH studies show.
The CDC stresses the need for a healthy weight and regular exercise to prevent Type 2 diabetes. These steps can greatly reduce the risk in high-risk groups.
Harvard School of Public Health research shows diet changes and an active lifestyle are vital for Type 2 diabetes prevention. It suggests reaching out to many people to teach them how to prevent it.
| Risk Factor | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Genetic predisposition | High | Moderate |
| Body weight | Not directly linked | Highly influential |
| Age of onset | Typically younger age | Often adults |
| Physical activity | Neutral | Critical preventive measure |
Diabetes Types Contrast: Monitoring and Management Strategies
Understanding and managing diabetes mellitus requires looking at how monitoring and treatment differ between Type 1 and Type 2. Both types affect how the body uses insulin. So, it’s key to have specific plans for each type to ensure good health.
Self-monitoring Blood Glucose Approaches
Checking blood sugar levels is a big part of managing diabetes. But, how often and how you do it can change a lot between types. People with Type 1 diabetes need to check their blood sugar often because they can’t make insulin. Those with Type 2 might not need to check as often, depending on their situation and treatment.
Comparing Medication Regimens in Diabetes Treatment
The treatments for Type 1 and Type 2 diabetes are quite different. This is because of how each type affects insulin in the body. Let’s look at a table that shows some common medicines for each type:
| Diabetes Type | Common Medications | Additional Treatment Considerations |
|---|---|---|
| Type 1 Diabetes | Insulin (multiple types) | Continuous glucose monitoring (CGM), insulin pumps |
| Type 2 Diabetes | Metformin, SGLT2 inhibitors, GLP-1 receptor agonists | Dietary adjustments, oral medications, non-insulin injectables |
This table shows a key diabetes mellitus comparison in treatments. Type 1 diabetes usually means taking insulin for life. Type 2 might use more medicines and also make lifestyle changes.
This way of managing diabetes helps control the disease better. It also shows how important it is to treat each type differently. By doing so, doctors can give better care and help people with diabetes live better lives.
Type 1 Diabetes vs Type 2 Diabetes: Associated Health Complications
Diabetes mellitus is a complex condition that affects health in different ways. It’s important to know the differences between Type 1 and Type 2 diabetes. This knowledge helps in managing and preventing health issues.
Acute Complications in Type 1 and Type 2 Diabetes
Acute health events show clear differences between Type 1 and Type 2 diabetes. Type 1 diabetes often leads to diabetic ketoacidosis (DKA), a dangerous acid buildup in the blood. Both types can experience low blood sugar, but the risks and treatments differ.
Chronic Health Issues and Their Relation to Diabetes Types
Long-term health effects of Type 1 and Type 2 diabetes also differ. Conditions like heart disease, nerve damage, kidney problems, and eye issues develop differently. These differences reflect the unique nature of each type of diabetes.
| Complication | Common in Type 1 | Common in Type 2 |
|---|---|---|
| Cardiovascular Disease | Less likely at onset, risk increases with age | More likely, influenced by lifestyle factors |
| Neuropathy | High risk, related to duration of diabetes | High risk, often correlated with obesity |
| Nephropathy | Progressive risk over years | Associated with high blood pressure |
| Retinopathy | Can develop rapidly | Increases with disease duration |
Using effective screening and prevention methods is key. Tailoring these to the type of diabetes is vital. Early action is critical in managing the disease, highlighting the need to understand the differences in complications.
Impact of Diabetes on Daily Life and Social Factors
Diabetes, whether type 1 or type 2, affects more than just health. By understanding diabetes types and the diabetes differences breakdown, we see how it touches daily life and social interactions.

Managing diabetes brings big challenges every day. People must change their diet, check blood sugar often, and take insulin if needed. These tasks can strain relationships and make work and social activities harder.
A study in Social Science & Medicine shows how diabetes can lead to misunderstandings. This affects personal and work relationships. It shows why we need to raise awareness and support for those with diabetes.
| Aspect | Impact on Type 1 Diabetes | Impact on Type 2 Diabetes |
|---|---|---|
| Daily Management | Constant monitoring, dietary restrictions, insulin dependency | Monitoring, diet control, exercise plans |
| Relationships | Need for significant support and understanding | Periodic support, lifestyle adjustment awareness |
| Workplace | Requires frequent breaks, possible stigma | Need for lifestyle integration, possible misunderstanding |
| Social Activities | Planning around medication schedule | Adapting activities to health needs |
The CDC talks about the big costs of diabetes, like more healthcare spending and lost work time. Teaching people about diabetes can help manage the disease better. This could lower some of these costs.
It’s key to build communities and workplaces that support people with diabetes. This understanding helps create a more inclusive society. It also helps in making better support and care for those with diabetes.
Technological Advancements in Diabetes Mellitus Management
Technology is changing how we manage diabetes, making life better for those with the disease. New tools like Continuous Glucose Monitoring (CGM) systems and advanced insulin delivery help tailor treatment. This approach effectively addresses the differences between type 1 and type 2 diabetes.
The Role of Continuous Glucose Monitoring
CGM systems are a big step forward in diabetes care, mainly for type 1 diabetes patients. Studies in The New England Journal of Medicine show they help keep blood sugar in check. These devices give real-time glucose readings, warning of highs or lows.
This constant data helps adjust treatment plans. It’s key for understanding and managing diabetes types.
Trends in Insulin Delivery Systems
Insulin delivery tech is getting better, making it easier to manage diabetes. The Endocrine Society journals talk about smart pens and pumps. These tools adjust doses and deliver insulin more evenly than old methods.
These advancements make daily life easier for diabetes patients. They bring us closer to more personalized and effective care.
Understanding the Emotional and Psychological Aspect of Diabetes
Diabetes affects more than just our bodies. It also impacts our mental health. The American Psychological Association (APA) and Diabetes Research and Clinical Practice have shown how diabetes can affect our emotions. This shows why treating diabetes fully means caring for our minds as well.
People with Type 1 Diabetes often feel anxious about needing insulin forever. Those with Type 2 Diabetes might stress about changing their lifestyle to manage their diabetes. These different feelings highlight the need to understand and compare diabetes types.
Diabetes distress is a term for the emotional struggles of managing diabetes. It affects both types of diabetes but needs different solutions. The APA and diabetes groups are working together. They’re using therapy and support groups to help with these mental health issues.
| Aspect | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Mental Health Challenge | Anxiety | Stress from lifestyle modifications |
| Common Emotional Response | Insulin dependency concerns | Diet and exercise pressure |
| Intervention Focus | Continuous support and monitoring | Behavioral adjustment support |
Studies show that custom care plans can greatly help diabetic patients’ mental health. Understanding these differences is key to better treatment and a better life for those with diabetes. So, it’s vital to look at diabetes from a whole-person perspective, treating both body and mind.
Diabetes Mellitus Variances: The Role of Healthcare Professionals
When we look at type 1 and type 2 diabetes, we see different challenges. Healthcare professionals play a key role in helping patients. They use their knowledge to give care that really makes a difference.
Endocrinologists, diabetes educators, and dietitians all have important jobs. They work together to help manage diabetes in different ways.
Endocrinologists and Their Role in Diabetes Care
Endocrinologists are key in diagnosing and treating diabetes. They create care plans that are just right for each patient. They use advanced tests to keep track of diabetes and adjust treatments as needed.
The Importance of Diabetes Educators and Dietitians
Diabetes educators and dietitians are very important. They teach patients about diabetes and help with meal planning. They make sure education and diet plans fit each patient’s needs.
Dietitians help patients with special diets for diabetes. This helps control blood sugar and improve health. Working together, healthcare professionals offer a strong support system for diabetes management.
Diabetes Contrast: Diet and Nutrition Guidelines
Understanding the diabetes mellitus comparison between type 1 and type 2 diets is key. The American Diabetes Association (ADA) has specific guidelines for each type. These guidelines meet the unique needs of each type.
Type 1 diabetes focuses on carbohydrate counting. This helps determine the right insulin dose for meals. It keeps blood sugar levels balanced. On the other hand, type 2 diabetes focuses on weight management and metabolic health. It suggests eating fewer calories and being more active.
The American Journal of Clinical Nutrition stresses the glycemic index and fiber intake. These help control blood sugar and manage weight. They show how different diabetes types have different nutritional needs.
The USDA dietary recommendations are a good starting point for diabetes-friendly eating. These guidelines can be adjusted to fit individual needs and health goals. They help manage each type of diabetes effectively.
- Carbohydrate counting and insulin dose adjustments for Type 1.
- Weight management strategies and calorie control for Type 2.
- Importance of glycemic index and fiber intake universally for diabetes management.
Using these tailored diets helps manage diabetes and improves life quality. It shows the importance of diet in diabetes mellitus comparison.
Staying Informed: Recent Research on Diabetes Differences Breakdown
Recent studies have shed light on the differences between type 1 and type 2 diabetes. Research in Diabetes, Metabolic Syndrome and Obesity is changing how we treat these diseases. It explores the molecular and genetic details that set them apart.
Every study brings us closer to personalized medicine. This means treatments that are more targeted and effective for each person with diabetes.
The Lancet Diabetes & Endocrinology has also made important discoveries. They’ve found key differences in the risk factors, symptoms, and how each type progresses. This knowledge helps doctors better manage these diseases.
It also helps patients understand their condition better. They can take steps to manage their diabetes more effectively.
There’s also progress in treatment options, as shown by The Journal of Clinical Investigation. New immune therapies for type 1 diabetes and new medications for type 2 offer hope. These breakthroughs show a future where treatments are tailored to each type of diabetes.
FAQ
Q: What are the main differences between type 1 and type 2 diabetes mellitus?
A: Type 1 diabetes is an autoimmune condition where the pancreas doesn’t make enough insulin. It’s often found in children. Type 2 diabetes is linked to insulin resistance and lifestyle choices. It usually happens in adults.
Q: How does diabetes mellitus impact metabolism?
A: Diabetes affects how the body uses and controls glucose. This can lead to high blood sugar levels. These levels can cause many health problems.
Q: What is the role of genetics and the environment in type 1 diabetes?
A: Genetics and viruses play a role in type 1 diabetes. While genes are important, viruses also trigger the autoimmune reaction that harms insulin-making cells.
Q: How do lifestyle factors influence the onset of type 2 diabetes?
A: Poor diet, lack of exercise, and obesity can cause insulin resistance. This is key in type 2 diabetes. Healthy choices can lower the risk of getting type 2 diabetes.
Q: Is there a difference in the age of onset between type 1 and type 2 diabetes?
A: Yes, type 1 diabetes usually starts in children and teens. Type 2 diabetes is more common in adults. But, type 2 is becoming more common in younger people too.
Q: What are the similarities and differences in the symptoms of type 1 and type 2 diabetes?
A: Both types can cause thirst, frequent urination, and tiredness. Type 1 symptoms come on fast and are severe. Type 2 symptoms take longer to show up, sometimes years.
Q: Why is insulin essential in managing type 1 diabetes, and how is it used differently in type 2 diabetes?
A: Insulin is key for type 1 diabetes because the body can’t make it. For type 2, insulin or other meds help control blood sugar when diet and exercise aren’t enough.
Q: Can type 2 diabetes be prevented?
A: Yes, you can lower your risk of type 2 diabetes with a healthy diet, exercise, and a healthy weight. There’s no known way to prevent type 1 diabetes.
Q: How do monitoring and management strategies vary between type 1 and type 2 diabetes?
A: Type 1 diabetes needs more frequent blood sugar checks and insulin management. Type 2 diabetes might use different meds, and monitoring needs vary based on the condition’s severity.
Q: What are the health complications associated with type 1 versus type 2 diabetes?
A: Both types can lead to serious problems like heart disease, kidney damage, and nerve damage. Type 1 can cause quick problems like diabetic ketoacidosis. Type 2 is linked to long-term issues like metabolic syndrome.
Q: How does diabetes affect daily life and social factors?
A: Diabetes requires daily care like blood sugar checks, meds, diet, and exercise. This can affect work, social life, and overall lifestyle. Living with diabetes can also have big social and mental impacts.
Q: What are some recent technological advancements in diabetes management?
A: New tech includes continuous glucose monitors, smart insulin pens and pumps, and the artificial pancreas. These tools help manage diabetes better.
Q: Are there psychological aspects of diabetes that differentiate type 1 from type 2?
A: Both types can lead to mental health issues like diabetes distress or depression. But, the experiences differ due to management needs and age of onset, with type 1 affecting younger people.
Q: What roles do healthcare professionals play in managing different types of diabetes?
A: Doctors, diabetes educators, and dietitians offer specialized care and education for diabetes. Their work is vital for both types, with approaches tailored to each condition’s needs.
Q: Do dietary and nutrition guidelines differ for individuals with type 1 versus type 2 diabetes?
A: Yes, both types need a balanced diet. Type 1 focuses on insulin management with carb counting. Type 2 emphasizes weight control and reducing insulin resistance.
Q: How does current research enhance the understanding of differences between type 1 and type 2 diabetes?
A: Research is ongoing to understand the biological differences between the two types. It aims to find new treatments and interventions. Studies focus on immune therapy for type 1 and new meds for type 2, each tailored to the specific disease mechanisms.

















