Breast cancer is a complex disease that affects millions of lives worldwide. This guide delves into the intricacies of breast cancer, from its early signs to advanced treatment options. We’ll explore the latest developments in oncology and discuss how metastasis impacts patient outcomes.
Whether you’re a patient, caregiver, or health-conscious individual, this guide aims to demystify breast cancer. We’ll cover essential topics like risk factors, screening methods, and cutting-edge therapies. By understanding these aspects, you’ll be better equipped to navigate the challenges of breast cancer or support those affected by it.
What is Breast Cancer: Definition and Basic Understanding
Breast cancer is a disease where cells in the breast grow out of control. It’s a common form of cancer, affecting millions worldwide. The disease starts when normal breast cells change and grow uncontrollably, forming a mass called a tumor.
Types of Breast Cancer Cells
Breast cancer can start in different parts of the breast. The two main types are:
- Ductal carcinoma: Starts in the milk ducts
- Lobular carcinoma: Begins in the milk-producing glands
Common Areas Where Breast Cancer Develops
Breast cancer often develops in specific areas of the breast:
- Milk ducts
- Lobules
- Connective tissue
How Cancer Cells Spread
Cancer cells can spread to other parts of the body through blood vessels or lymph nodes. This process is called metastasis. When breast cancer spreads, it’s known as metastatic breast cancer. Common sites for breast cancer metastasis include bones, liver, lungs, and brain.
| Stage | Description |
|---|---|
| Early-stage | Cancer confined to breast |
| Advanced | Cancer spread beyond breast |
| Metastatic | Cancer spread to distant organs |
Understanding breast cancer is key for early detection and effective treatment. Regular screenings and awareness of risk factors are important in managing this disease.
Early Warning Signs and Symptoms of Breast Cancer
Knowing the early signs of breast cancer can save lives. Regular self-exams and professional screenings are key. They help find this disease early. Being aware of symptoms lets you act fast if something seems wrong.
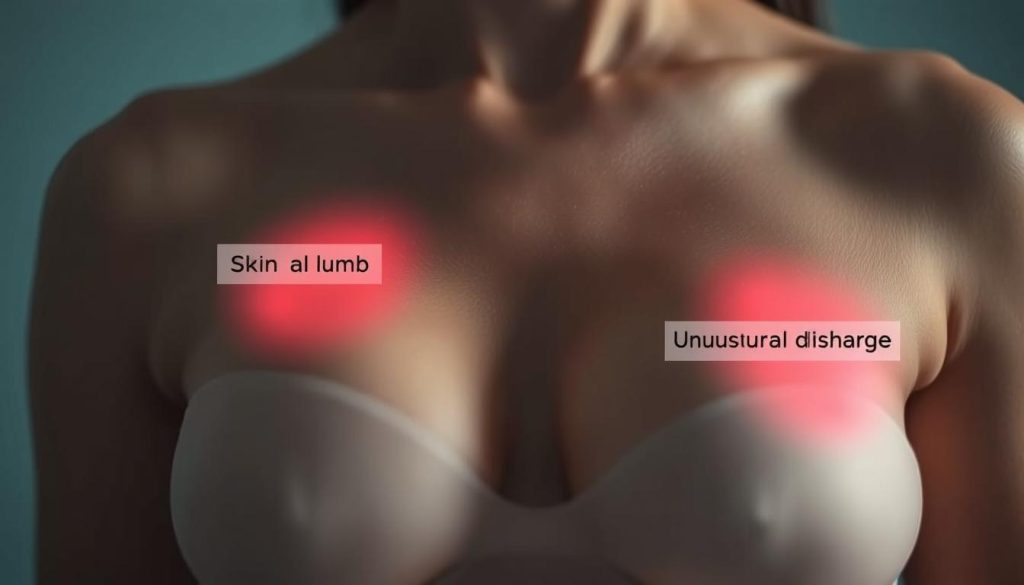
- A new lump or thickening in the breast or armpit area
- Changes in breast size, shape, or appearance
- Skin changes, such as dimpling or redness
- Nipple changes, including inversion or discharge
- Unexplained breast pain
These signs don’t always mean cancer. But, it’s best to see a doctor if you notice any changes. Understanding the early warning signs and symptoms of breast cancer empowers you to take charge of your health.
While self-exams are helpful, they don’t replace mammograms. These X-ray images can spot breast changes before you feel them. The American Cancer Society suggests yearly mammograms for women 45 and older. Some may need to start earlier based on their risk factors.
Remember, early detection often leads to better outcomes. Stay vigilant about your breast health. Don’t hesitate to seek medical advice if something worries you.
Risk Factors and Common Causes
Knowing about breast cancer risk factors is key to prevention and early detection. Some risks are beyond our control. Others can be changed by our lifestyle choices.
Genetic Predisposition
Genes like BRCA1/BRCA2 are very important in breast cancer risk. If these genes mutate, the risk of breast cancer goes up a lot. Women with BRCA1 mutations face a 55-65% chance of breast cancer by age 70. BRCA2 mutations raise the risk to 45%.
Lifestyle and Environmental Factors
Our lifestyle choices can impact breast cancer risk. Drinking alcohol, not exercising, and being overweight are all factors. Exposure to radiation or chemicals can also play a part.
| Lifestyle Factor | Risk Increase |
|---|---|
| Alcohol (2-3 drinks daily) | 20% |
| Obesity (post-menopausal) | 30-60% |
| Lack of exercise | 10-20% |
Age and Gender Considerations
Age is a big risk factor for breast cancer. Most cases happen in women over 50. Women are 100 times more likely to get breast cancer than men. As women get older, regular screenings become more important, even more so for those with extra risk factors.
Breast Cancer Screening Methods and Guidelines
Breast cancer screening is key to finding cancer early. This can lead to better treatment results. Regular checks can spot cancer before symptoms show up.

- Mammograms: X-ray images of the breast that can detect tumors before they’re felt
- Clinical breast exams: Physical examinations performed by healthcare professionals
- Breast self-exams: Regular self-checks to familiarize yourself with your breast tissue
- Breast MRI: Magnetic resonance imaging for high-risk individuals
- Ultrasound: Sound wave imaging to complement mammograms
Guidelines say mammograms are the best first choice. The American Cancer Society advises annual mammograms for women 45-54. Starting at 40 is also an option.
Women 55 and older can choose biennial or annual screenings. It depends on what they prefer or their health needs.
| Age Group | Recommended Screening | Frequency |
|---|---|---|
| 40-44 | Optional mammogram | Annual |
| 45-54 | Mammogram | Annual |
| 55+ | Mammogram | Annual or Biennial |
Women with higher risk factors might need more frequent or earlier checks. It’s important to talk to your doctor. They can help figure out the best screening plan for you.
The Importance of Regular Mammograms
Regular mammograms are key for catching breast cancer early. They can spot tumors before they grow, helping with treatment.
When to Start Mammogram Screenings
Health groups say start mammograms at 40. But, if you’re at higher risk, you might need to start sooner. Talk to your doctor about when to start.
Different Types of Mammography
Breast cancer screening has changed. Here are the main types of mammograms:
- 2D Digital Mammography: The usual screening method
- 3D Mammography (Tomosynthesis): Gives clearer images
- Contrast-Enhanced Mammography: Uses dye for better views
Understanding Mammogram Results
You’ll get a BI-RADS score after your mammogram. This score shows how likely cancer is.
| BI-RADS Category | What It Means | Follow-up Action |
|---|---|---|
| 0 | Incomplete | More imaging needed |
| 1 | Negative | Keep up with routine screening |
| 2 | Benign | Keep up with routine screening |
| 3 | Probably benign | Short-term follow-up |
| 4 | Suspicious | Biopsy suggested |
| 5 | Highly suggestive of malignancy | Biopsy needed |
Remember, mammograms are a key part of breast cancer screening. Regular check-ups can save lives by finding cancer early.
Diagnostic Procedures and Testing
Getting a correct breast cancer diagnosis is key for good treatment. Doctors use different methods to find out if cancer is there and what to do next. These steps help figure out the exact type and how far it has spread.

Imaging tests are very important in finding breast cancer. Mammograms, ultrasounds, and MRIs show detailed pictures of the breast. They can spot areas that need more checking. Doctors might use special dyes to make tumors stand out better.
Biopsies are a must for a clear diagnosis. A small piece of breast tissue is taken out for a closer look. There are a few types of biopsies:
- Fine-needle aspiration: Uses a thin needle to get cells
- Core needle biopsy: Takes out a small piece of tissue
- Surgical biopsy: Removes a bigger piece of tissue
Pathologists look at the biopsy samples under a microscope. They check if there are cancer cells. They also figure out the tumor’s type and grade. This helps doctors plan the best treatment.
Genetic testing is getting more important too. It looks for genes like BRCA1 and BRCA2 that raise cancer risk. Knowing this helps doctors choose the right treatment and prevention steps.
Blood tests are also used in diagnosis. They check for tumor markers and overall health. As breast cancer diagnosis gets better, patients get more tailored and accurate care.
Understanding Breast Cancer Stages
Knowing the stage of breast cancer is key to planning treatment. Doctors use breast cancer stages to describe how far the disease has spread. This helps them choose the best care plan for each patient.
TNM Staging System
The TNM system is the main way to stage breast cancer. It looks at three things:
- T: Tumor size
- N: Lymph node involvement
- M: Metastasis (spread to other parts of the body)
Stage Descriptions
Breast cancer stages range from 0 to IV:
| Stage | Description |
|---|---|
| 0 | Non-invasive cancer cells in breast ducts |
| I | Small tumor, no lymph node spread |
| II | Larger tumor or limited lymph node spread |
| III | Larger tumor with more lymph node spread |
| IV | Cancer has spread to other parts of the body |
Metastatic Breast Cancer
Stage IV breast cancer is called metastatic. This means the cancer has spread beyond the breast and nearby lymph nodes to other parts of the body. Common sites for metastasis include bones, liver, lungs, and brain. While stage IV breast cancer is serious, new treatments are helping people live longer with a good quality of life.
Treatment Options and Approaches
Breast cancer treatment has many options, each tailored to the patient’s needs. The choice depends on the cancer’s stage, type, and what the patient prefers. Let’s look at the main ways to fight this disease.
Surgery Options: Lumpectomy vs. Mastectomy
Surgery is often the first step against breast cancer. There are two main surgeries: lumpectomy and mastectomy. A lumpectomy takes out the tumor and some tissue around it. A mastectomy removes the whole breast. Your doctor will choose the best surgery for you.
Radiation Therapy Protocols
Radiation therapy kills cancer cells with high-energy beams. It’s used after surgery to get rid of any left-over cancer cells. The treatment lasts several weeks, with daily sessions. Side effects can include skin irritation and feeling tired.
Chemotherapy Treatment Plans
Chemotherapy uses drugs to kill cancer cells all over the body. It can be used before surgery to make tumors smaller or after to lower the chance of cancer coming back. Chemo is given in cycles, with breaks in between.
| Treatment | Purpose | Duration | Common Side Effects |
|---|---|---|---|
| Lumpectomy | Remove tumor | 1-2 hours | Pain, swelling |
| Mastectomy | Remove entire breast | 2-3 hours | Pain, lymphedema |
| Radiation Therapy | Kill remaining cancer cells | 3-6 weeks | Skin irritation, fatigue |
| Chemotherapy | Destroy cancer cells | 3-6 months | Nausea, hair loss |
Your treatment plan might include one or more of these options. Your healthcare team will work with you to make a plan that’s just right for you.
Targeted Therapies and Immunotherapy
Breast cancer treatment has made big strides in recent years. Oncology experts now use targeted therapies and immunotherapy to fight specific breast cancer types. These new methods bring hope and better results for patients.
Targeted therapies aim at specific molecules that help cancer grow. They block these molecules, which slows or stops cancer. Targets include HER2 proteins and hormone receptors.
Immunotherapy, on the other hand, strengthens the body’s immune system to fight cancer. It teaches the immune system to find and attack cancer cells. This method has shown great promise in some breast cancer types.
| Treatment Type | How It Works | Common Side Effects |
|---|---|---|
| HER2-targeted therapy | Blocks HER2 proteins on cancer cells | Heart problems, nausea |
| CDK4/6 inhibitors | Slow cancer cell growth | Fatigue, low blood cell counts |
| Immune checkpoint inhibitors | Boost immune response against cancer | Skin rash, flu-like symptoms |
These treatments usually have fewer side effects than traditional chemotherapy. They can be used alone or with other treatments. Your oncologist will choose the best option for you based on your cancer type and stage.
Hormone Therapy for Breast Cancer
Hormone therapy is a key part of treating breast cancer, mainly for hormone receptor-positive tumors. It targets cancer cells that grow because of hormones. This method helps slow or stop their growth.
Types of Hormone Treatments
Doctors have several hormone therapy options for breast cancer:
- Selective estrogen receptor modulators (SERMs)
- Aromatase inhibitors
- Estrogen receptor downregulators
- Luteinizing hormone-releasing hormone agonists
Each type works in its own way to lower hormone levels or block their impact on cancer cells. Your oncologist will pick the best one for you, based on your cancer type and stage.
Side Effects Management
Hormone therapy can cause side effects, like hot flashes, mood swings, and bone loss. To help, your care team might suggest:
- Regular exercise to keep bones strong
- Dietary changes for better health
- Medications for specific symptoms
Talking openly with your healthcare provider is important during hormone therapy for breast cancer. They can adjust your treatment to reduce discomfort and ensure the best results.
Recovery and Rehabilitation Process
The journey to recovery after breast cancer goes beyond just finishing treatment. Patients face both physical and emotional challenges as they heal and adjust to life after cancer. Oncology experts help guide them through this important time, focusing on rebuilding strength and improving overall health.
Physical rehab often includes exercises to improve mobility and lower the risk of lymphedema. Many survivors work with physical therapists to create recovery plans tailored to them. These plans aim to boost range of motion, reduce fatigue, and enhance fitness.
Emotional healing is just as critical in breast cancer recovery. Support groups, counseling, and mindfulness can help manage anxiety, depression, and fear of cancer coming back. Oncology teams often provide mental health resources, knowing how important they are for long-term recovery.
Nutritional advice is also a key part of rehab. Eating a balanced diet helps the body heal and may prevent cancer from coming back. Many oncology centers offer nutrition counseling to help patients make healthy food choices during and after treatment.
As survivors move forward in their recovery, they often find new strength and resilience. Many say they appreciate life more and have stronger bonds with their loved ones. While the journey is tough, with the right support and care, people can do well after breast cancer treatment.
Living with Breast Cancer: Emotional Support
Coping with breast cancer is not just about physical treatment. Emotional support is key to healing. Support groups and mental health care are vital in oncology care. They help patients face challenges.

Support Groups and Resources
Breast cancer support groups offer a safe place for patients to share and find comfort. They provide valuable resources, advice, and emotional connections. Hospitals and oncology centers often host meetings, both in-person and online.
- Local breast cancer organizations
- Online forums and chat rooms
- Survivor-led support networks
- Family and caregiver support groups
Mental Health Care During Treatment
Oncology teams know mental health is critical in breast cancer treatment. Many hospitals now offer mental health services. These services help with anxiety, depression, and stress from diagnosis and treatment.
| Mental Health Service | Benefits |
|---|---|
| Individual counseling | Personalized coping strategies |
| Art therapy | Creative expression of emotions |
| Mindfulness meditation | Stress reduction and relaxation |
| Psychiatric consultation | Medication management if needed |
Emotional support during breast cancer treatment greatly improves life quality and treatment results. Patients should talk about mental health with their oncology team. They should also explore available resources for full care.
Prevention Strategies and Lifestyle Changes
We can’t stop all breast cancers, but we can lower our risk. Experts in oncology suggest several lifestyle changes. Eating a diet full of fruits, veggies, and whole grains is a good start. Also, exercising for at least 150 minutes a week is beneficial.
Drinking less alcohol is also important. Even a little can raise your risk. It’s best to drink in moderation or not at all. Knowing how hormones work is key too. If you’re thinking about hormone therapy or birth control, talk to your doctor first.
Other ways to prevent include staying at a healthy weight, mainly after menopause. Avoiding harmful chemicals is also good. If you have a high risk because of family history or genes, your doctor might suggest more tests or medicines. These steps don’t promise to prevent cancer, but they can greatly reduce your risk and improve your health.
FAQ
Q: What are the early warning signs of breast cancer?
A: Early signs of breast cancer include a lump or thickening. You might also notice changes in breast size or shape. Skin dimpling, nipple inversion, nipple discharge, or persistent pain are other signs.
It’s important to do regular self-exams. If you see any unusual changes, talk to a healthcare professional right away.
Q: How often should I get a mammogram?
A: How often you need a mammogram depends on your age and risk factors. Women aged 45-54 should get one every year. Those 55 and older can switch to getting one every two years.
But, if you’re at higher risk, you might need to start sooner or get more frequent screenings. Always check with your doctor for what’s best for you.
Q: What’s the difference between a lumpectomy and a mastectomy?
A: A lumpectomy removes the tumor and some tissue but keeps most of the breast. A mastectomy removes the whole breast. The choice depends on the tumor’s size, location, and cancer stage.
Q: How does radiation therapy work in treating breast cancer?
A: Radiation therapy uses beams to kill cancer cells and shrink tumors. It’s often used after surgery to kill any remaining cancer cells. This helps lower the chance of cancer coming back.
The treatment is given in daily sessions for several weeks. It targets the area where the tumor was.
Q: What are the side effects of chemotherapy for breast cancer?
A: Chemotherapy can cause hair loss, nausea, and fatigue. It can also make you more likely to get infections and change your appetite. These side effects can be tough but are usually temporary.
Your oncology team will help you manage these side effects. They’ll work with you to make your treatment as comfortable as possible.
Q: What is metastatic breast cancer?
A: Metastatic breast cancer, or Stage IV, means cancer has spread to other parts of the body. This can include the bones, lungs, liver, or brain. While it’s not curable, there are treatments to help manage symptoms and extend life.
Q: How do BRCA1 and BRCA2 gene mutations affect breast cancer risk?
A: BRCA1 and BRCA2 mutations greatly increase the risk of breast and ovarian cancer. Women with these mutations have a 45-65% chance of getting breast cancer by age 70. The general risk is about 12%.
Genetic testing can find these mutations. This allows for early screening and preventive steps.
Q: What lifestyle changes can help reduce the risk of breast cancer?
A: To lower your risk, stay at a healthy weight and exercise often. Limit alcohol and avoid smoking. Eat a diet full of fruits and vegetables.
Try to breastfeed and use hormone replacement therapy only when necessary. Regular screenings and self-exams are key for early detection.
Q: How does hormone therapy work in treating breast cancer?
A: Hormone therapy blocks or lowers hormones that can grow hormone-receptor-positive breast cancers. This can be done with medications like tamoxifen or by removing the ovaries in premenopausal women. The right treatment depends on your menopausal status and cancer type.
Q: What support resources are available for breast cancer patients?
A: Many support resources are out there, like local and online groups, counseling, and organizations like the American Cancer Society and Susan G. Komen Foundation. They offer emotional support, advice, and educational materials.
Many hospitals also have breast cancer support programs. These help patients during their treatment journey.


















