Pancreatic cancer is a serious disease that affects many lives each year. It includes different types of pancreatic neoplasms. We will look into the details of pancreatic cancer, from early signs to treatment options.
We will discuss the types of pancreatic tumors and risk factors. We will also talk about how to diagnose it. We’ll share the latest research and offer support for those living with pancreatic cancer.
Learning about pancreatic cancer helps us fight it better. Let’s start this journey together. We aim to shed light on this often hidden disease.
What is Pancreatic Cancer: An Overview of Pancreatic Neoplasms
Pancreatic cancer is a serious disease that affects thousands of Americans each year. It happens when cells in the pancreas grow out of control, forming tumors. Knowing the basics of this condition is key for early detection and treatment.
The Structure and Function of the Pancreas
The pancreas is a vital organ behind the stomach. It makes enzymes for digestion and hormones like insulin to control blood sugar. When tumors form, they mess with these important functions.
Types of Pancreatic Tumors
Pancreatic tumors can be benign or malignant. The most common type is pancreatic adenocarcinoma, which starts in the cells lining the pancreatic ducts. Other types include neuroendocrine tumors and cystic neoplasms.
| Tumor Type | Origin | Frequency |
|---|---|---|
| Pancreatic Adenocarcinoma | Exocrine cells | 85% |
| Neuroendocrine Tumors | Endocrine cells | 5% |
| Cystic Neoplasms | Various cell types | 10% |
Risk Factors and Prevalence
Several factors increase the risk of pancreatic cancer. These include smoking, obesity, diabetes, and a family history of the disease. In the United States, pancreatic cancer is the third leading cause of cancer-related deaths. Early detection and awareness of risk factors are key to improving outcomes for those affected by this challenging disease.
Early Warning Signs and Symptoms of Pancreatic Cancer
Spotting the early signs of pancreatic cancer can be tough. But it’s key for catching it early. Many symptoms seem vague or not related at first. Knowing these signs can help find cancer sooner, leading to better treatment.
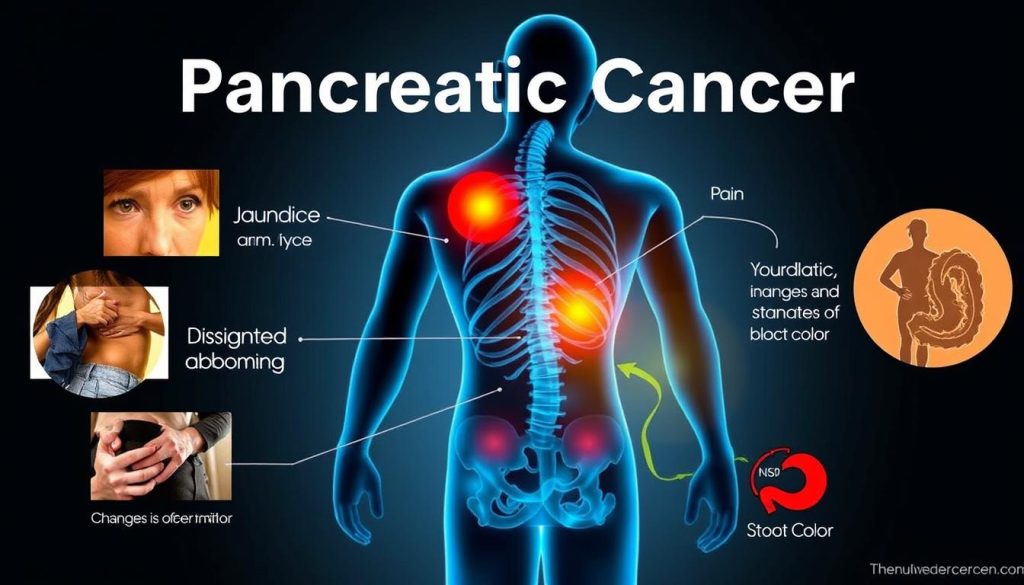
- Abdominal pain that radiates to the back
- Unexplained weight loss
- Jaundice (yellowing of skin and eyes)
- Loss of appetite
- Changes in stool color or consistency
- New-onset diabetes, specially in older adults
These symptoms can also mean other health issues. If you keep feeling these symptoms, see your doctor for a check-up.
| Symptom | Description | When to Seek Medical Attention |
|---|---|---|
| Abdominal Pain | Pain in the upper abdomen that may spread to the back | If pain lasts more than a few days |
| Jaundice | Yellowing of skin and whites of eyes | Right away if you notice it |
| Weight Loss | Unintentional weight loss without diet or exercise changes | If you lose more than 5% of body weight in 6-12 months |
Finding pancreatic cancer early can change treatment and outcomes. If you see any of these signs, get medical help. While these signs don’t always mean cancer, it’s safer to check your health.
Common Risk Factors for Developing Pancreatic Malignancies
Knowing what increases your risk of pancreatic ductal adenocarcinoma can help prevent and detect it early. Let’s look at the main risk factors for this serious condition.
Genetic Predisposition
Some people are born with a higher risk of pancreatic cancer due to their genes. If your family has a history of this disease, talk to your doctor about genetic testing.
- BRCA1 and BRCA2 mutations
- Lynch syndrome
- Familial atypical multiple mole melanoma syndrome
Lifestyle Factors
Your daily habits can greatly affect your cancer risk. Making healthy choices can lower your risk of pancreatic ductal adenocarcinoma.
| Risk Factor | Impact on Pancreatic Cancer Risk |
|---|---|
| Smoking | Doubles the risk |
| Obesity | 20% increased risk |
| Heavy alcohol use | 1.5 times higher risk |
Medical Conditions
Certain health issues can increase your risk of pancreatic ductal adenocarcinoma. If you have these conditions, it’s key to work closely with your healthcare team:
- Chronic pancreatitis
- Diabetes (long-standing type 2)
- Cirrhosis of the liver
By understanding these risk factors, you can take steps to protect your health and catch any problems early. Remember, having risk factors doesn’t mean you’ll get pancreatic cancer. But it’s wise to stay informed and proactive about your well-being.
Diagnosis Methods for Pancreatic Ductal Adenocarcinoma
Finding pancreatic exocrine tumors early is key to good treatment. Doctors use many ways to spot these tumors. Let’s look at the main ways to find pancreatic cancer.
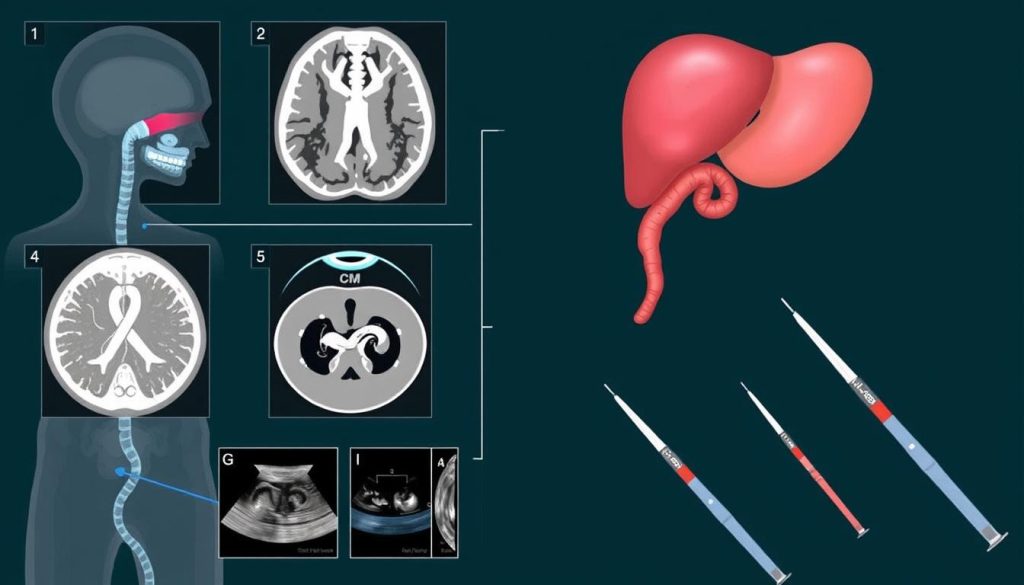
Imaging studies are very important in finding pancreatic exocrine tumors. CT scans and MRIs give clear pictures of the pancreas. They help doctors find any odd growths. Endoscopic ultrasound gives a close look at the pancreas, helping find tumors accurately.
Blood tests can also help find pancreatic cancer. These tests look for certain substances that might show cancer. While not perfect, they give clues for more checks.
Biopsy procedures give the clearest sign of pancreatic cancer. Doctors take a small piece of tissue from the tumor. They look at it under a microscope to see if it’s cancer.
| Diagnostic Method | Purpose | Accuracy |
|---|---|---|
| CT Scan | Visualize pancreas and surrounding areas | High |
| MRI | Detailed soft tissue imaging | High |
| Endoscopic Ultrasound | Close-up view of pancreas | Very High |
| Blood Tests | Detect cancer markers | Moderate |
| Biopsy | Confirm cancer presence | Definitive |
Using these methods together helps doctors find pancreatic exocrine tumors well. Finding them early can lead to better treatment and outcomes.
Understanding Different Stages of Pancreatic Cancer
Pancreatic cancer staging is key to figuring out treatment plans and what to expect. The stage tells us how far the cancer has spread. This includes pancreatic islet cell tumors, which are less common but just as important to grasp.
Stage I and II: Early-Stage Disease
In these early stages, the cancer stays within the pancreas. Stage I tumors are under 2 cm, while Stage II tumors are bigger or have reached nearby lymph nodes. Treatment usually starts with surgery to remove the tumor, followed by chemotherapy.
Stage III: Locally Advanced Disease
At this stage, the cancer has grown beyond the pancreas and might involve nearby blood vessels. It hasn’t reached distant parts of the body yet. Treatment may include chemotherapy, radiation, and sometimes surgery.
Stage IV: Metastatic Disease
In Stage IV, the cancer has spread to distant organs like the liver or lungs. This includes metastatic pancreatic islet cell tumors. Treatment aims to manage symptoms and slow cancer growth. Chemotherapy is the main treatment, with targeted therapies for certain tumors.
Knowing these stages helps both patients and doctors make better treatment choices. Remember, each case is different, and pancreatic islet cell tumors may act differently than other pancreatic cancers.
Traditional Treatment Options for Pancreatic Tumors
Pancreatic cancer treatment often involves a mix of approaches. Doctors tailor these treatments to each patient’s specific case, including rare forms like pancreatic acinar cell carcinoma. Let’s explore the main traditional options available.
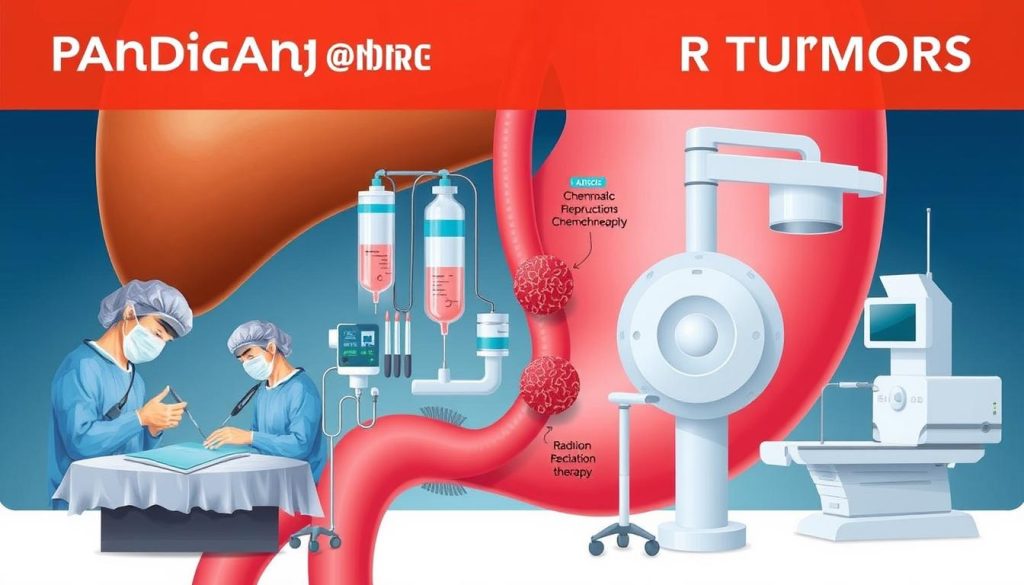
Surgery is a key treatment for many pancreatic tumors. It aims to remove the cancerous tissue when possible. For pancreatic acinar cell carcinoma, surgical removal can be an effective option if caught early.
Chemotherapy uses powerful drugs to kill cancer cells throughout the body. It’s often used before or after surgery, or as the main treatment when surgery isn’t an option. Specific drug combinations may be used for pancreatic acinar cell carcinoma.
Radiation therapy targets cancer cells with high-energy beams. It can shrink tumors before surgery or help manage symptoms in advanced cases. For pancreatic acinar cell carcinoma, radiation may be combined with chemotherapy for better results.
| Treatment | Purpose | Use in Pancreatic Acinar Cell Carcinoma |
|---|---|---|
| Surgery | Remove tumor | Primary option if localized |
| Chemotherapy | Kill cancer cells | Often combined with surgery |
| Radiation | Shrink tumors | Used with chemo for better outcomes |
These traditional treatments form the backbone of pancreatic cancer care. Your doctor will create a plan that best suits your specific diagnosis and overall health condition.
Surgical Procedures for Pancreatic Exocrine Tumors
Surgery is key in treating pancreatic exocrine tumors, like pancreatic mucinous neoplasms. These surgeries aim to remove cancerous tissue. This can greatly improve patient outcomes. Let’s look at the main surgical options available.
Whipple Procedure
The Whipple procedure is a common surgery for pancreatic cancer. It removes the head of the pancreas, part of the small intestine, gallbladder, and bile duct. This complex surgery is often used for tumors in the head of the pancreas.
Distal Pancreatectomy
For tumors in the body or tail of the pancreas, a distal pancreatectomy is performed. This surgery removes the left side of the pancreas and sometimes the spleen. It’s used for smaller tumors in these areas.
Total Pancreatectomy
In some cases, removing the entire pancreas is needed. This is called total pancreatectomy. It’s done when tumors are widespread or there are multiple tumors. While it removes the cancer risk, it leads to diabetes and requires lifelong enzyme replacement.
| Procedure | Parts Removed | Common Indications |
|---|---|---|
| Whipple | Head of pancreas, part of small intestine, gallbladder, bile duct | Tumors in pancreatic head |
| Distal Pancreatectomy | Left side of pancreas, sometimes spleen | Tumors in body or tail |
| Total Pancreatectomy | Entire pancreas | Widespread tumors or multiple neoplasms |
Chemotherapy Protocols for Pancreatic Cancer Treatment
Chemotherapy is a key treatment for pancreatic neoplasms. It uses powerful drugs to kill cancer cells throughout the body. Doctors choose from several chemotherapy protocols based on the cancer stage and patient health.
FOLFIRINOX is a common first-line treatment for advanced pancreatic cancer. This protocol combines four drugs: fluorouracil, leucovorin, irinotecan, and oxaliplatin. It’s known for its effectiveness but can cause significant side effects.
For patients who can’t tolerate FOLFIRINOX, gemcitabine plus nab-paclitaxel is often used. This combination has shown improved survival rates compared to gemcitabine alone. Some doctors use gemcitabine as a single agent for older or weaker patients.
| Protocol | Drugs | Typical Use |
|---|---|---|
| FOLFIRINOX | Fluorouracil, Leucovorin, Irinotecan, Oxaliplatin | Advanced pancreatic neoplasms |
| Gemcitabine + Nab-paclitaxel | Gemcitabine, Nab-paclitaxel | Alternative to FOLFIRINOX |
| Gemcitabine alone | Gemcitabine | Older or less fit patients |
Side effects of chemotherapy can include fatigue, nausea, hair loss, and increased risk of infections. Doctors work closely with patients to manage these effects and maintain quality of life during treatment.
Radiation Therapy Approaches for Pancreatic Adenocarcinoma
Radiation therapy is key in treating pancreatic tumors. It uses high-energy beams to target cancer cells and shrink tumors. For patients with pancreatic adenocarcinoma, this treatment is often combined with other therapies to improve outcomes.
External Beam Radiation
External beam radiation is a common approach for pancreatic tumors. A machine outside the body directs radiation to the tumor site. Treatment sessions are brief, lasting 10 to 30 minutes. Patients usually receive treatments five days a week for several weeks.
This method can help shrink tumors before surgery or relieve symptoms in advanced cases.
Stereotactic Body Radiation Therapy
Stereotactic body radiation therapy (SBRT) is a newer, more precise technique. It delivers high doses of radiation to pancreatic tumors in fewer sessions. SBRT uses advanced imaging to pinpoint the tumor’s location.
This allows for higher doses with less damage to surrounding healthy tissue. Patients may complete treatment in just one to five sessions. SBRT can be effective for small, localized pancreatic tumors or when surgery isn’t an option.
Both methods aim to destroy cancer cells while sparing healthy tissue. Your doctor will recommend the best approach based on your specific case. Factors like tumor size, location, and overall health play a role in this decision. Radiation therapy can significantly improve quality of life for many patients with pancreatic tumors.
Innovative Treatments and Clinical Trials
The fight against pancreatic cancer is moving forward with new therapies. Researchers are finding new ways to fight this tough disease. This brings hope to patients and their families.
Immunotherapy is leading the way in new treatments. It uses the body’s immune system to attack cancer cells. Trials are testing drugs like checkpoint inhibitors and CAR-T cell therapy for pancreatic cancer.

Targeted therapies are also showing promise. These drugs aim at specific genetic changes in tumors. For example, PARP inhibitors might help those with BRCA gene mutations.
Scientists are looking into new ways to deliver drugs. One idea uses nanoparticles to carry chemotherapy right to the tumors. This could make treatments more effective and reduce side effects.
| Innovative Treatment | Description | Current Stage |
|---|---|---|
| Immunotherapy | Activates immune system to fight cancer | Phase II/III clinical trials |
| Targeted Therapy | Attacks specific genetic mutations | FDA approved for certain patients |
| Nanoparticle Drug Delivery | Delivers drugs directly to tumors | Early-stage clinical trials |
These new treatments for pancreatic cancer offer hope. While some are in trials, they mark important progress. They show a strong fight against this tough disease.
Managing Pancreatic Islet Cell Tumors
Pancreatic islet cell tumors are different from pancreatic ductal adenocarcinoma. They start from hormone-making cells in the pancreas. They need special care because of this.
Diagnosis Approaches
There are several ways to find pancreatic islet cell tumors:
- Blood tests to check hormone levels
- Imaging studies like CT scans and MRIs
- Endoscopic ultrasound for detailed pancreas views
- Biopsy to confirm tumor type
It’s important to find these tumors early. Pancreatic neuroendocrine tumors can cause symptoms. These symptoms help doctors find the tumors.
Treatment Strategies
The treatment for pancreatic islet cell tumors depends on several factors:
- Surgery to remove the tumor
- Targeted therapy to block tumor growth
- Hormone therapy to manage symptoms
- Chemotherapy for advanced cases
- Radiation therapy to shrink tumors
Islet cell tumors usually have a better outlook than pancreatic ductal adenocarcinoma. Researchers are working hard to make treatments better. They want to improve life for patients with these rare tumors.
Supportive Care and Pain Management
Living with pancreatic cancer is tough, but supportive care makes a big difference. It helps improve patients’ quality of life. Pain management is a big focus, as many patients feel discomfort.
Doctors use medicines, nerve blocks, or other methods to control pain. This helps patients feel more comfortable.
Nutrition support is also key. The disease can mess with digestion and appetite. Working with a dietitian to create a personalized eating plan is important.
Some patients need enzyme supplements to help digest food better. This helps them keep their strength and energy up.
Emotional and psychological support is just as important. Many hospitals offer counseling and support groups. These help patients and their families deal with the stress and anxiety of a pancreatic cancer diagnosis.
Palliative care teams focus on managing symptoms and improving quality of life. They work with oncologists to address physical, emotional, and spiritual needs. This ensures patients get care that goes beyond just treating the cancer.
FAQ
Q: What is pancreatic cancer?
A: Pancreatic cancer is a disease where cancer cells grow in the pancreas. It includes different types, with pancreatic ductal adenocarcinoma being the most common. This cancer often grows quietly, making it hard to catch early.
Q: What are the early warning signs of pancreatic cancer?
A: Early signs include stomach pain, yellow skin and eyes, unexplained weight loss, and changes in appetite. Stool color or consistency changes can also be a sign. These symptoms often show up when the cancer is already advanced.
Q: Who is at risk for developing pancreatic cancer?
A: Risk factors include age over 45, smoking, obesity, and diabetes. Chronic pancreatitis and certain genetic conditions also increase risk. But, having risk factors doesn’t mean you’ll get cancer. Some people with pancreatic cancer have no known risk factors.
Q: How is pancreatic cancer diagnosed?
A: Diagnosis uses imaging tests like CT scans and MRIs, blood tests, and sometimes a biopsy. Genetic testing may also be done, depending on the type of tumor or family history.
Q: What are the treatment options for pancreatic cancer?
A: Treatment depends on the cancer’s stage and type. It may include surgery, chemotherapy, or radiation. For pancreatic ductal adenocarcinoma, a team approach is often used. New treatments like targeted therapies and immunotherapies are being tested.
Q: What is the Whipple procedure?
A: The Whipple procedure is a surgery for pancreatic cancer in the head of the pancreas. It removes the head of the pancreas, part of the small intestine, the gallbladder, and the bile duct. It’s used for treating some types of pancreatic cancer.
Q: What is the survival rate for pancreatic cancer?
A: Survival rates vary by stage and type of tumor. Pancreatic cancer is often detected late, which lowers survival rates. But, early-stage cancer that’s removed surgically has a better chance. Remember, survival rates are averages, and individual results can differ.
Q: Are there any new treatments being developed for pancreatic cancer?
A: Yes, researchers are exploring new treatments. They focus on targeted therapies, immunotherapies, and personalized medicine. Clinical trials are ongoing, giving hope for better treatments in the future.
Q: How can I manage pain associated with pancreatic cancer?
A: Pain management includes medications, nerve blocks, and radiation therapy. Complementary therapies like acupuncture or meditation can also help. A pain specialist or palliative care team can create a plan tailored to you.
Q: What support resources are available for pancreatic cancer patients and their families?
A: Many resources are available, like patient groups, online forums, and local support groups. They offer emotional support, advice, and connections. Cancer centers also provide counseling, nutrition guidance, and financial help. Ask your healthcare team about resources in your area.