Dealing with sacroiliac joint dysfunction can be tough. It affects many people, causing ongoing pain but often goes unnoticed. We aim to shed light on the many SI joint pain causes.
Our mission is to give expert insights on SI joint pain. It’s not just about helping you feel better. It’s about giving you the tools to find relief and move forward with confidence.
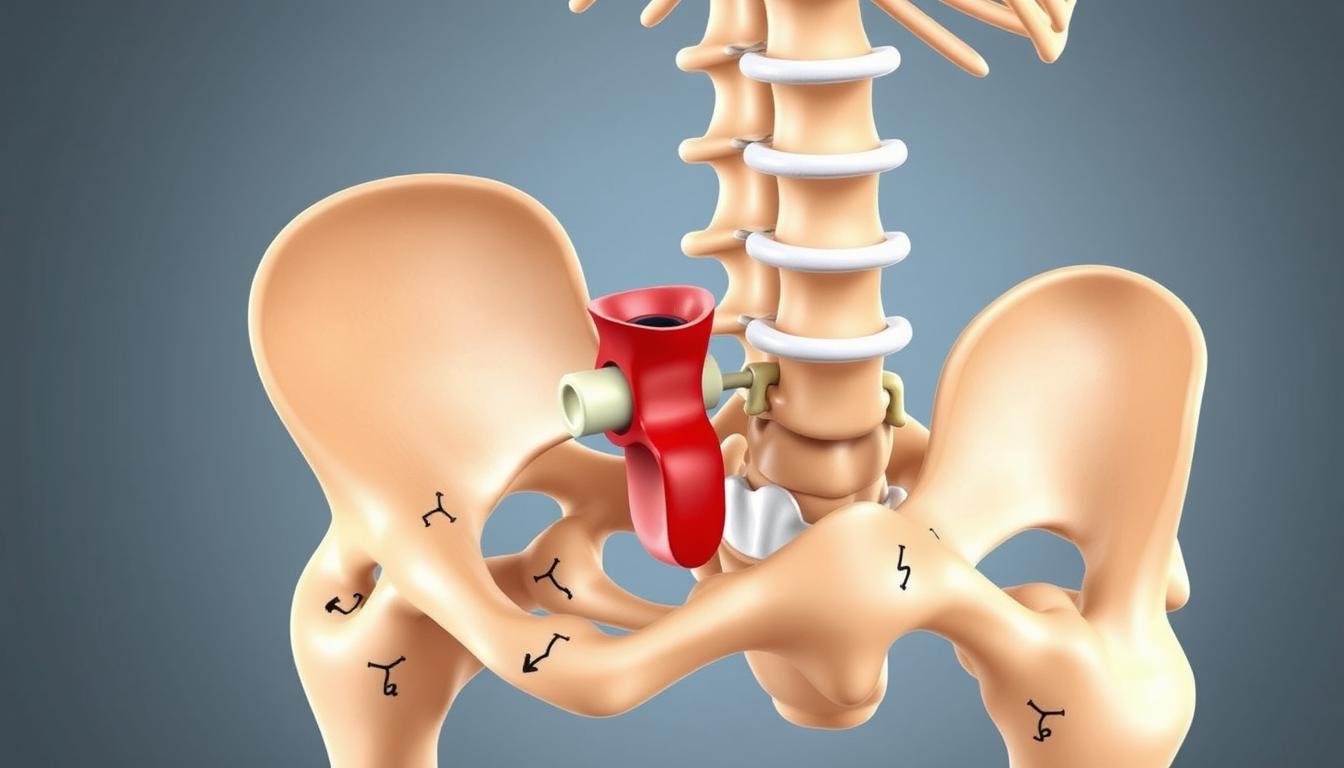
What is the SI Joint and its Function in the Body?
The SI joint, or sacroiliac joint, is a key part of the pelvis. It sits where the sacrum meets the iliac bones. This joint is important for both stability and movement, helping us do daily tasks without back pain.
Anatomy of the Sacroiliac Joint
The SI joint has the surfaces of the sacrum and iliac bones. These are connected by strong ligaments and covered in cartilage. This setup helps the joint handle forces and movements from the lower spine to the pelvis and legs, keeping us stable.
Role of the SI Joint in Movement and Stability
Knowing how the SI joint moves and supports the body is key to solving back pain. Its limited but important movement helps spread the body’s weight evenly. This balance is vital for standing, walking, and protecting the lower spine from too much stress.
Learning more about the SI joint and its role can help treat chronic back pain. Keeping this joint healthy is important for better movement and spinal health.
| Movement Type | Impact on SI Joint |
|---|---|
| Flexion/Extension | Modulates pressure distribution across the joint |
| Rotation | Limited rotation helps maintain pelvic stability |
| Lateral Bending | Distributes mechanical stress, reducing spinal load |
Comprehensive Overview of SI Joint Pain Causes
It’s important to know why Sacroiliac (SI) joint pain happens. This pain can come from pelvic instability, trauma-induced pain, and inflammatory conditions. We’ll look at each of these to understand how they cause SI joint pain.
- Pelvic Instability: This is often caused by physical activities or hormonal changes. It can make the SI joint unstable, leading to pain and discomfort.
- Trauma-Induced Pain: Accidents or sudden impacts can hurt the SI joint. This pain is usually very bad and needs quick medical help.
- Inflammatory Conditions: Arthritis or ankylosing spondylitis can make the SI joints inflamed. This causes long-term pain and makes it hard to move.
SI joint pain is hard to treat because it has many causes. Doctors need to understand how these causes work together to find the right treatment.
Here’s how these factors can make SI joint pain worse:
| Cause | Common Symptoms | Possible Treatments |
|---|---|---|
| Pelvic Instability | Uneven gait, hip pain, lower back pain | Physical therapy, pelvic braces |
| Trauma-Induced Pain | Immediate sharp pain, swelling, decreased range of motion | Ice application, rest, anti-inflammatory medications |
| Inflammatory Conditions | Chronic dull ache, stiffness in the morning | Anti-inflammatory drugs, corticosteroid injections |
Differentiating SI Joint Pain from Other Types of Back Pain
Finding the source of back pain can be tricky. Sacroiliac (SI) joint pain and issues with the lumbar spine often cause pain in the same area. This makes it important to tell them apart. Doctors use specific symptoms and tests to figure out the real cause of pain.
Comparison with Lumbar Spine Issues
Lumbar spine problems include things like herniated discs and spinal stenosis. These issues affect the lower back but are different from SI joint pain. Knowing the differences is key to treating them right.
- Lumbar pain often goes down to the legs and feet, while SI joint pain stays in the buttock or lower spine area.
- Activities like bending, twisting, and lifting make lumbar spine issues worse. But SI joint pain can get worse even with simple actions like standing up from sitting.
- Morning stiffness is more common in lumbar conditions and gets better with movement. SI joint pain doesn’t change as much during the day.
Identifying Characteristics of SI Joint Pain
Spotting SI joint pain is key to effective treatment. Symptoms include:
- Sharp, stabbing pain at the spine and pelvis junction.
- Pain gets worse when standing up from sitting or climbing stairs.
- Pain is on one side of the body or feels like the legs are unstable.
Understanding these unique signs helps doctors treat SI joint pain differently from lumbar spine issues. This way, they can give the right treatment for each patient’s back pain.
Pelvic Instability and its Contribution to Sacroiliac Dysfunction
Pelvic instability is a key factor in sacroiliac dysfunction, which often causes lower back pain. This condition happens when the pelvis doesn’t stay in its right place. It affects the sacroiliac joints, which are between the sacrum and iliac bones.
Pelvic instability messes with the pelvis’s normal balance. This can put too much stress on the sacroiliac joints. This stress can make sacroiliac dysfunction worse or start it, causing pain and trouble moving.
- The laxity of ligaments in the pelvic area, which can be due to hormonal changes, injury, or genetic factors, often leads to instability.
- Uneven weight distribution or prolonged stress due to postural habits or occupational demands can further strain the sacroiliac joints.
- Muscular imbalances surrounding and supporting the pelvis and hip region can lead to asymmetric forces being applied to the sacroiliac joints.
People with sacroiliac dysfunction or lower back pain need to know about pelvic instability. The table below shows the difference between stable and unstable pelvises. It helps understand the symptoms and risks of each:
| Condition | Symptoms | Potential Complications |
|---|---|---|
| Stable Pelvis | Minimal or no pain, normal mobility | Lower risk of joint dysfunction |
| Unstable Pelvis | Chronic back pain, difficulty walking | Higher risk of sacroiliac dysfunction |
This comparison shows why fixing pelvic instability early is important. It can stop sacroiliac dysfunction from getting worse. Getting the right treatment can make life better and lower back pain less common.
Understanding How Inflammatory Conditions Affect the SI Joint
Inflammatory conditions, like chronic or autoimmune ones, greatly affect the SI joint. They cause inflammation and discomfort. Knowing how these conditions impact the sacroiliac joint is key to managing SI joint pain.
Autoimmune Factors Leading to SI Joint Inflammation
Autoimmune factors are a big reason for SI joint inflammation. Diseases like ankylosing spondylitis and rheumatoid arthritis make the immune system attack the joints. This leads to ongoing inflammation, affecting movement and quality of life.
Understanding these autoimmune factors is vital. It helps in finding treatments that fight the inflammation at its root.
The Impact of Chronic Inflammatory Conditions
Chronic inflammatory conditions make SI joint inflammation worse. They keep the inflammation going, causing more stiffness and pain. Conditions like psoriatic arthritis not only harm the skin but also the joints, making treatment harder.
Dealing with these conditions needs a wide range of treatments. This includes medicines to reduce inflammation, physical therapy to keep joints moving, and sometimes surgery. For more on how these conditions can lead to serious issues like bone marrow edema, check out this resource.
| Condition | Impact on SI Joint | Treatment Approach |
|---|---|---|
| Ankylosing Spondylitis | Severe inflammation leading to joint fusion | Biologics, NSAIDs |
| Rheumatoid Arthritis | Chronic inflammation with joint degradation | DMARDs, physical therapy |
| Psoriatic Arthritis | Joint inflammation with skin symptoms | Systemic treatments, topical therapies |
The Role of Trauma in Triggering SI Joint Pain
It’s key to know how trauma affects the sacroiliac (SI) joint to find the cause of pain. Both sudden injuries and long-term stress can cause problems in this important area. We’ll look at how different traumas impact the SI joint, focusing on sudden injuries and long-term stress.
Acute Injuries and Their Consequences
Acute injuries happen suddenly and can severely harm the SI joint. Examples include falls, sports injuries, and car accidents. These events can cause immediate pain and make it hard to move.
Chronic Trauma and Repetitive Stress Injuries
Repetitive stress injuries come from constant strain on the SI joint. Activities that repeat the same motion can cause ongoing irritation. This is common in athletes, dancers, and people who do repetitive tasks at work.
| Injury Type | Description | Impact on SI Joint |
|---|---|---|
| Acute Traumatic Events | Includes falls, collisions, and accidents. | Immediate, intense pain and possible long-term joint problems. |
| Repetitive Stress | Continuous strain from overuse or wrong use. | Pain builds up slowly, leading to long-term issues. |
Looking into trauma, both sudden and ongoing, shows why it’s vital to find and treat the root of SI joint pain. By understanding these complex issues, we can find better ways to treat pain and help joints work better.
Pregnancy-Related SI Joint Pain and Pelvic Changes
During pregnancy, the body changes a lot. Pelvic changes and lower back pain are common. These issues often come from pregnancy-related SI joint pain.
This pain is mainly due to hormonal changes. These changes make ligaments softer, getting ready for childbirth.
The sacroiliac joint in the lower back is affected. It’s connected to the pelvis by strong ligaments. As pregnancy goes on, the joint feels more stress because of the growing weight and changed balance.
This stress can cause pain not just in the pelvis but also in the lower back. This is known as lower back pain.
- Increased hormone levels lead to ligament laxity, altering pelvic stability.
- The growing uterus shifts the center of gravity, increasing strain on the SI joints.
- Changes in posture and gait in response to the body’s new dynamics can exacerbate stress on the SI joint.
It’s important to understand these changes to manage pregnancy-related SI joint pain. Doctors suggest several ways to help. These include prenatal yoga to strengthen the pelvic muscles and maternity belts for support.
Age-Related Degeneration as a Factor in SI Joint Pain
As we get older, our bodies change in ways that can affect our health and how we move. The sacroiliac (SI) joint in our lower back is one area that changes with age. It helps our upper body and legs work together, keeping us balanced and mobile.
With time, the SI joint wears down, losing cartilage. This loss of cartilage is a big reason for SI joint pain. As we age, this problem gets worse, making older adults more likely to have SI joint issues. We’ll look at how these changes cause pain and what can help.
- Natural wear and tear due to repetitive motion and prolonged pressure over the years
- Dry-up of lubricating joint fluid, leading to increased friction and pain
- Stiffening of the ligaments surrounding the joint, which hampers flexibility and movement
By focusing on these issues, we can reduce some of the pain from SI joint degeneration.
| Age Group | Symptoms Experienced | Recommended Interventions |
|---|---|---|
| 50-60 years | Mild to moderate stiffness and pain | Physical therapy, moderate exercise |
| 61-70 years | Moderate to severe stiffness and pain | Enhanced physical therapy, pain medication |
| Over 70 years | Severe stiffness and pain, mobility issues | Comprehensive pain management, possible surgical consultation |
Knowing how age-related degeneration leads to SI joint pain helps us find better ways to live with it. This approach can help manage symptoms and keep us moving well.
Exploring the Link Between Piriformis Syndrome and SI Joint Pain
The connection between Piriformis syndrome and the sacroiliac (SI) joint is key to understanding lower back pain. Knowing how these issues work together helps find better ways to manage pain for those who suffer from it.
Defining Piriformis Syndrome
Piriformis syndrome happens when the piriformis muscle in the buttock presses on the sciatic nerve. This can cause pain, tingling, or numbness in the buttocks and down the leg. It’s a muscle and nerve problem, but it can also affect nearby areas like the SI joint.
Interaction Between the Piriformis Muscle and the SI Joint
The piriformis muscle and the SI joint are close together. When the piriformis muscle is tight or spasms, it can change how the pelvis moves. This can hurt the SI joint, making pain worse or similar to SI joint problems. This creates a complex pattern of pain in the pelvis.
| Condition | Symptoms | Impact on SI Joint |
|---|---|---|
| Piriformis Syndrome | Muscle spasms, buttock pain, sciatica | Can alter pelvic alignment, contributing to SI joint misalignment and pain |
| SI Joint Dysfunction | Lower back pain, pain in groin, hip, and buttocks | Directly affects pelvic stability, influencing gait and posture |
Investigating the Relationship Between SI Joint Pain and Sciatica
The connection between sacroiliac (SI) joint pain and sciatica is complex. It often puzzles both patients and doctors. Symptoms of SI joint dysfunction can look a lot like sciatica, making diagnosis tricky.
Understanding Sciatica and its Symptoms
Sciatica causes pain that spreads along the sciatic nerve. This nerve runs from the lower back to the hips and down each leg. Sciatica usually affects one side of the body.
Its symptoms include numbness, tingling, or weakness in the leg or foot. The pain can range from a mild ache to sharp, burning, or severe pain.
How SI Joint Dysfunction Can Mimic Sciatica
SI joint dysfunction symptoms can include pain in the lower back and hips. This pain can also be felt on one side of the body, similar to sciatica. It might spread to the buttocks and thighs, causing confusion with true sciatica.
A key difference is that SI joint pain is usually more focused around the joint. This is unlike the wide spread of sciatic pain.
Looking into these overlapping areas shows the need for careful diagnosis. It also shows how spinal and pelvic structures are connected. Problems in one can greatly affect the other.
SI Joint Pain Causes: A Critical Look at Prevalent Triggers
Looking into the SI joint pain causes is key for good treatment. This part talks about the prevalent triggers that make SI joint pain worse. It’s important for finding the right diagnosis.
These causes come from many places, like how we move and changes in our body. Here’s a detailed look at these triggers:
- Mechanical stress: Standing or sitting for too long puts extra pressure on the SI joint, causing pain.
- Biomechanical inefficiencies: Bad posture or walking can really strain the SI joint.
- Trauma: Getting hurt or having an injury can make the joint and muscles around it unstable, leading to long-term pain.
- Pregnancy: Hormonal changes and how weight shifts during pregnancy affect the SI joint a lot.
These things, alone or together, can really hurt how well the SI joint works and stays stable.
| Trigger | Description | Impact Level |
|---|---|---|
| Mechanical Stress | Long periods of standing or sitting put continuous pressure on the SI joint. | High |
| Biomechanical Inefficiencies | Poor body mechanics, such as improper lifting techniques and abnormal posture. | Medium |
| Trauma | Injuries from accidents or falls that directly impact the lower back and pelvic area. | High |
| Pregnancy | Relaxation of ligaments and added weight can destabilize the SI joint. | Variable |
Knowing these prevalent triggers is key to making treatment plans that really work. It’s all about meeting the needs of each person with SI joint pain causes.
How Hormonal Fluctuations Can Lead to SI Joint Pain
Hormonal changes affect the body, including the SI joint’s stability. The SI joint, where the spine meets the pelvis, needs strong ligaments to stay stable. Hormones like relaxin and estrogen change during puberty, menstruation, pregnancy, and menopause. These changes can weaken the ligaments, causing SI joint pain.
During pregnancy, relaxin makes the pelvic area more flexible for childbirth. This flexibility can make the SI joints less stable, leading to pain. Estrogen changes during menstruation and menopause also weaken SI joint ligaments. This makes the area more prone to pain and inflammation.
| Life Stage | Hormone Involved | Effect on SI Joint |
|---|---|---|
| Puberty | Estrogen | Initial exposure can temporarily destabilize SI joint |
| Menstruation | Estrogen fluctuations | Recurrent weakening of ligaments leading to periodic SI joint pain |
| Pregnancy | Relaxin | Significant loosening of ligaments, increasing SI joint mobility and pain |
| Menopause | Decreasing Estrogen | Chronic weakening of SI joint ligaments, heightening pain risk |
Hormonal fluctuations are a natural part of life. But knowing how they affect the SI joint can help prevent and manage SI joint pain. This is very important for women going through hormonal changes due to their menstrual cycles, pregnancy, or menopause.
Lifestyle and Environmental Factors Influencing SI Joint Health
The health of the sacroiliac (SI) joint is greatly affected by lifestyle and environmental factors. It’s important to know how our daily activities, work, and surroundings impact our SI joint. Understanding these factors helps us prevent and manage SI joint pain.
Occupation-Related Risks for SI Joint Dysfunction
Jobs that involve heavy lifting or long hours of sitting or standing can harm the SI joint. For example, construction workers or those who use heavy machinery often face more pressure on their SI joints. This highlights the need for ergonomic practices and safety measures at work.
Impact of Exercise and Physical Activity Levels
Exercise is key to keeping the SI joint stable and healthy. Regular physical activities strengthen the muscles around the joint, supporting it. On the other hand, a lack of exercise or wrong workout routines can weaken the joint, leading to pain. It’s best to mix strength training, core exercises, and flexibility workouts for the best results.
- Strength training aids in building the muscles necessary for joint support.
- Core exercises enhance stability and protect the SI joint from irregular movements.
- Flexibility workouts maintain joint and muscle health, preventing stiffness.
Non-Surgical Interventions for Managing SI Joint Pain
Looking into non-surgical ways to handle Sacroiliac (SI) joint pain is smart and safe. These methods help ease pain, boost function, and keep you healthy for the long haul. They avoid the risks of surgery.
Physical Therapy Techniques
Physical therapy is key in treating SI joint pain without surgery. Therapists use hands-on techniques to work on and strengthen the area. They teach exercises to build muscle, improve core strength, and stretch tight ligaments.
This helps support the SI joint better and cuts down stress on it.
Alternative Therapies and their Efficacy
Along with physical therapy, other treatments help manage SI joint pain. Acupuncture, yoga, and chiropractic care are among them. They all help by improving movement and easing pain.
Each therapy has its own way of reducing inflammation and fixing alignment without surgery.
| Therapy | Description | Benefits |
|---|---|---|
| Acupuncture | Uses fine needles at specific body points | Reduces pain, enhances circulation |
| Yoga | Focuses on posture, flexibility, and breathing | Increases flexibility, decreases stress on joints |
| Chiropractic Care | Employs spinal manipulation and alignment techniques | Improves spinal posture, reduces nerve irritability |
Each therapy is customized for the person’s symptoms and health. They aim to ease pain and enhance life quality through non-surgical interventions. It’s vital to talk to a healthcare expert to find the right treatment. This ensures it’s done right and safely.
When to Consider Surgery for Chronic SI Joint Pain
If you’re dealing with long-lasting pain in your sacroiliac joint, surgery might be an option. This choice comes after trying other treatments like physical therapy and medicine. When these don’t help, and pain keeps you up at night, it’s time to think about surgery.
Talking to your doctor about the risks and benefits of surgery is key. They can help you understand if it’s right for you.
Surgery for sacroiliac joint pain offers different types of treatments. Some are less invasive, like SI joint fusion. This surgery stops the joint from moving, which can help with pain.
It’s important to know about the different surgeries and what they mean for you. Your doctor will check if surgery is a good choice. They’ll look at your health and how damaged the joint is.
How well you recover from surgery can vary. But, many people find their pain goes down and they can do more things. After surgery, you’ll need to follow a rehabilitation plan. This is important for a good outcome.
Deciding to have surgery is a big step. But, for many, it’s a chance for lasting relief from chronic pain.
FAQ
Q: What are the main causes of SI joint pain?
A: SI joint pain can come from several sources. This includes sacroiliac joint dysfunction and pelvic instability. Issues in the lumbar spine, trauma, and arthritis are also common causes. Age and pregnancy can also play a role.
Q: How does the SI joint function in the body?
A: The SI joint connects the spine to the pelvis. It’s key for movement and stability. It helps absorb shock and distribute weight.
Q: How can I differentiate SI joint pain from other types of lower back pain?
A: SI joint pain feels sharp and stabbing in the lower back or buttocks. It can spread to the legs. It’s different from other back pain because of its location and how it changes with movement.
Q: What is pelvic instability and how does it relate to SI joint dysfunction?
A: Pelvic instability means the pelvis doesn’t support or move right. This can put too much strain on the SI joint. This strain can cause dysfunction and pain.
Q: Can physical activity and lifestyle impact SI joint health?
A: Yes, your job, how active you are, and your exercise habits can affect your SI joint. Too little or too much activity can cause problems.
Q: What are some non-surgical interventions for managing SI joint pain?
A: Non-surgical treatments include physical therapy to strengthen muscles. Manual manipulation and alternative therapies like acupuncture or chiropractic care are also options.
Q: When is surgery considered for SI joint pain?
A: Surgery is considered when other treatments haven’t worked. It aims to stabilize the joint and reduce pain.
Q: What role does trauma play in SI joint pain?
A: Trauma, like falls, can cause SI joint pain. So can chronic trauma from repetitive activities. This can lead to inflammation and damage.
Q: How do hormonal fluctuations contribute to SI joint pain?
A: Hormonal changes can make the pelvis’s ligaments relax. This reduces stability and increases the risk of SI joint pain. This is seen during menstrual cycles, pregnancy, and menopause.
Q: Can SI joint pain be related to Piriformis syndrome or Sciatica?
A: Yes. Piriformis syndrome can make SI joint pain worse. It irritates the sciatic nerve near the SI joint. SI joint dysfunction can also mimic sciatica, causing leg pain and numbness.
Go to the full page to view and submit the form.