Testicular cancer is a common male reproductive cancer that affects thousands yearly. This guide covers the basics, from early detection to treatment. We aim to give you the knowledge to help save lives.
Spotting testicular cancer early is key to better treatment. We’ll look at symptoms, risk factors, and how it’s diagnosed. Our goal is to give you clear, useful info to tackle testicular cancer.
We’ll discuss treatments like surgery and radiation therapy. By the end, you’ll know a lot about testicular cancer and how to stay healthy.
What Is Testicular Cancer and Its Prevalence
Testicular cancer is a serious health issue that mainly affects young men. It starts in the testicles, which make sperm and testosterone. Knowing about it helps find and treat it early.
Definition and Types of Testicular Cancer
Testicular cancer, or testicular tumor, is a growth in the testicles. There are two main types: seminoma and nonseminoma. Seminomas grow slowly and respond well to radiation. Nonseminomas grow faster and need more treatment.
Both types start from the cells that make sperm. They are called germ cell tumors.
Statistical Data in the United States
In the U.S., testicular cancer is rare but serious. About 9,000 new cases are found each year. It’s the most common cancer in young men.
The good news is that most men survive if caught early. Over 95% live five years after diagnosis.
Age Groups Most Affected
Young and middle-aged men are most at risk. The average age of diagnosis is 33. But it can happen at any age.
Men between 15 and 35 are at the highest risk. So, it’s important for them to check themselves regularly.
| Age Group | Risk Level | Percentage of Cases |
|---|---|---|
| 15-35 | Highest | 50% |
| 35-50 | Moderate | 30% |
| 50+ | Low | 20% |
Early Warning Signs and Symptoms
Spotting testicular cancer symptoms early is key to successful treatment. Signs of male reproductive cancer often start quietly. It’s important for men to watch for changes in their testicles and the area around them.
A painless lump or swelling in either testicle is the most common sign of testicular cancer. This lump can be as small as a pea or much bigger. Some men also feel a heavy or aching feeling in their lower abdomen or scrotum.
- Sudden fluid buildup in the scrotum
- Pain or discomfort in a testicle or the scrotum
- Enlargement or tenderness of the breasts
- Back pain, which may indicate spread to lymph nodes
Not all lumps are cancerous. Some might be from infections or other issues. Regular self-exams help men get to know their body. This way, they can spot changes fast.
If you see any unusual changes or symptoms that won’t go away, get medical help right away. Catching testicular cancer early greatly improves treatment success and survival chances. Remember, many signs of male reproductive cancer are subtle. Trust your gut and see a doctor if you’re worried.
Risk Factors for Developing Testicular Tumors
Knowing about testicular cancer risk factors is key to catching it early. Some risks we can’t change, but knowing them helps us make better choices and see doctors sooner.
Genetic Predisposition
Genetics play a big part in testicular cancer. Men with a family history are at higher risk. Certain genes, like the KITLG gene, make it more likely.
Environmental Risk Factors
Environmental factors can also raise testicular cancer risk. Some chemicals, found in certain jobs, can increase risk. Smoking is another lifestyle choice that can raise risk levels.
Medical History Considerations
Medical history matters too. Men with undescended testicles or abnormal growths are at higher risk. Infections or injuries to the testicles can also raise risk.
| Risk Factor | Impact Level | Preventable |
|---|---|---|
| Family History | High | No |
| Undescended Testicles | Moderate | Treatable |
| Chemical Exposure | Variable | Yes |
Understanding these risk factors helps us take care of our health. Regular self-checks and talking to doctors are important. They help catch testicular cancer early and treat it well.
The Biology of Germ Cell Tumors
Germ cell tumors are key in understanding testicular cancer. They start in cells that make sperm, called germ cells. Knowing about them helps us understand testicular cancer better.
Germ cell tumors are mainly seminomas and non-seminomas. Seminomas grow slowly and stay in the testes. Non-seminomas spread fast and affect younger men. Sometimes, a tumor can be both, making treatment harder.
These tumors start with DNA changes in germ cells. These changes can come from genetics or the environment. As cells keep dividing wrong, they form a mass that can spread to other tissues.
- Seminomas: Usually found in men aged 30-50
- Non-seminomas: Often affect men in their 20s and 30s
- Mixed germ cell tumors: Contain both types
Studying how these tumors grow and spread is part of testicular cancer biology. Germ cell tumors can release proteins into the blood. Doctors use these markers to find and track the disease. This knowledge helps in making better treatments and improving patient care.
Diagnostic Methods and Testing
Diagnosing testicular cancer involves several steps to find and stage the disease. Finding it early is key to successful treatment. Let’s look at the main ways doctors diagnose it.
Physical Examination Procedures
Doctors first do a thorough physical exam. They feel for lumps or swelling in the testicles. They also check for big lymph nodes in the groin. This hands-on check helps spot any issues that need more looking into.
Imaging Studies
Imaging tests are key for diagnosing testicular cancer. Ultrasounds give detailed images of the testicles, spotting any odd masses. CT scans and PET scans help see if the cancer has spread, guiding treatment plans.
Blood Tests and Tumor Markers
Blood tests look for specific tumor markers linked to testicular cancer. These markers show if cancer is present and help track treatment. The main markers are:
| Tumor Marker | Description | Significance |
|---|---|---|
| Alpha-fetoprotein (AFP) | Protein made by liver cells and yolk sac tumors | Shows up in some testicular cancers |
| Human chorionic gonadotropin (HCG) | Hormone made by placental tissue | Often high in testicular germ cell tumors |
| Lactate dehydrogenase (LDH) | Enzyme in body tissues | Shows tissue damage, high in advanced cancer |
These tests work together to give a full picture. This helps doctors create a treatment plan that fits each patient’s needs.
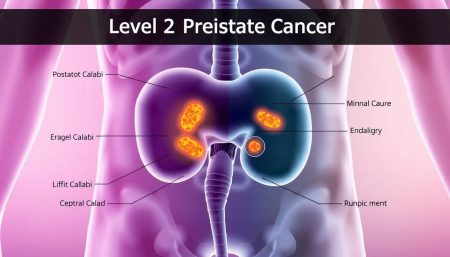
Stages of Testicular Cancer
Understanding testicular cancer stages is key for effective treatment. Doctors use a staging system to see how far the cancer has spread. This helps them plan the best treatment.
- Stage 1: Cancer is confined to the testicle
- Stage 2: Cancer has spread to nearby lymph nodes
- Stage 3: Cancer has spread beyond lymph nodes to other parts of the body
Each stage has substages based on tumor growth and affected organs. Stage 1 is early-stage disease with a high cure rate. Stage 2 means the cancer has spread regionally. Stage 3 is more advanced.
Oncologists use tests like blood work, imaging studies, and sometimes surgery to determine the stage. The stage of testicular cancer is important for choosing the right treatment. Treatments may include surgery, chemotherapy, or radiation therapy.
Early detection through regular self-exams can lead to diagnosis at lower stages. This increases the chances of successful treatment. If you notice any unusual changes in your testicles, see a healthcare provider right away.
Treatment Options for Testicular Cancer
Testicular cancer treatment has many options, each tailored to the patient. Urologic oncology specialists work with patients to find the best plan.
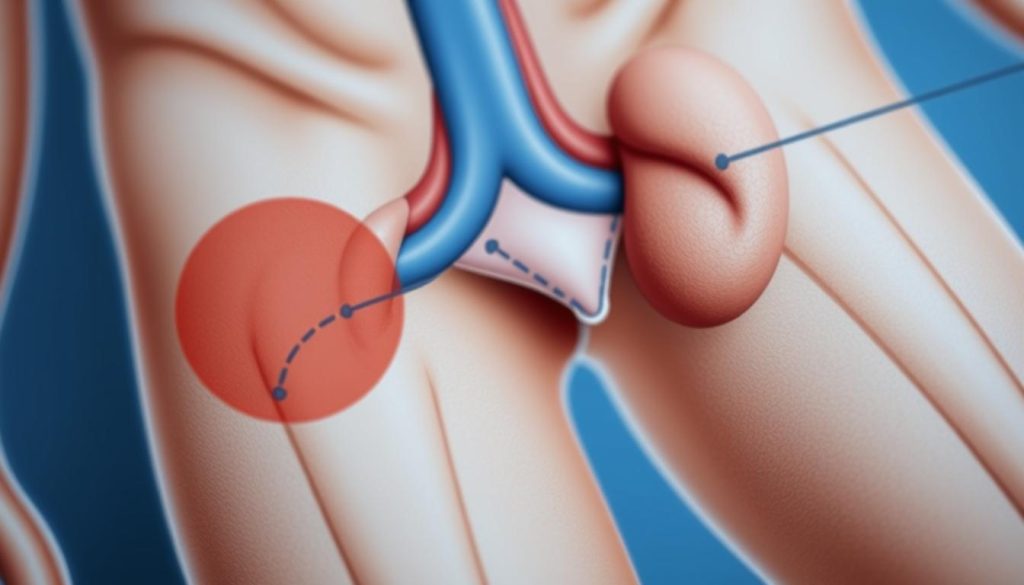
Surgery and Orchiectomy
The main treatment for testicular cancer is orchiectomy. This surgery removes the affected testicle. It’s often the first step and helps confirm the diagnosis.
Radiation Therapy Protocols
Radiation therapy kills cancer cells with high-energy beams. It’s mainly used for seminoma-type testicular cancers. Treatment sessions are short but happen over several weeks.
Chemotherapy Regimens
Chemotherapy fights cancer cells all over the body. It’s key for advanced stages or when cancer spreads. Common drugs include cisplatin, etoposide, and bleomycin.
| Treatment | Main Use | Duration |
|---|---|---|
| Orchiectomy | All cases | One-time surgery |
| Radiation | Early-stage seminoma | 2-3 weeks |
| Chemotherapy | Advanced stages | 9-12 weeks |
Your urologic oncology team will guide you through each step. They ensure you get the right care for your case.
The Role of Urologic Oncology Specialists
Urologic oncology specialists are key in managing testicular cancer. They focus on cancers of the urinary system and male reproductive organs. Their deep knowledge helps them give top-notch care for testicular tumors.

These specialists lead a team to create personalized treatment plans. They work with surgeons, radiologists, and oncologists for complete care. This teamwork ensures the best outcomes for patients.
Urologic oncology experts use the latest techniques for diagnosis and treatment. They keep up with new advancements in oncological treatment. Their expertise covers all aspects of care, from diagnosis to long-term follow-up.
| Responsibilities | Skills |
|---|---|
| Diagnosis and staging | Advanced imaging interpretation |
| Treatment planning | Surgical expertise |
| Surgical procedures | Knowledge of latest therapies |
| Post-treatment care | Patient communication |
Patients greatly benefit from the care of urologic oncology experts. These specialists treat the cancer and address concerns about fertility and quality of life. Their holistic approach ensures patients get full support during their cancer journey.
Recovery and Rehabilitation Process
The journey to recover from testicular cancer is long and requires careful steps. It involves post-surgery care, physical healing, and emotional support. Patients go through a big change that needs patience and help from doctors.
Post-Surgery Care
After orchiectomy, patients must follow certain care steps. They need to keep the incision clean, manage pain with medicine, and avoid hard activities. Testicular cancer recovery often starts with a short hospital stay and then rest at home.
Physical Recovery Timeline
The time it takes to recover physically varies. Most can start with light activities in 1-2 weeks after surgery. But, full recovery might take 4-8 weeks. This depends on how much treatment they had, like chemotherapy or radiation.
| Recovery Stage | Timeline | Activities Allowed |
|---|---|---|
| Initial Recovery | 1-2 weeks | Light walking, rest |
| Intermediate Stage | 2-4 weeks | Daily routines, light exercise |
| Full Recovery | 4-8 weeks | Normal activities, work resumption |
Emotional Support and Counseling
Emotional healing is key in testicular cancer recovery. Many find help in counseling and support groups. These help with body image, fertility, and fear of cancer coming back. Doctors often include mental health support in the treatment plan.
Fertility Preservation Options

Men with testicular cancer often worry about their future family plans. Fertility preservation gives them hope to become dads later. It involves saving reproductive material before treatment starts.
Sperm banking is the main fertility preservation method for these patients. It’s a simple process where men give a semen sample to freeze and store. This works for those who can naturally produce sperm.
For those who can’t ejaculate, doctors have other ways to collect sperm:
- Testicular sperm extraction (TESE)
- Microsurgical epididymal sperm aspiration (MESA)
- Electroejaculation
These methods help preserve fertility even when cancer impacts sperm or ejaculation. It’s key for men with testicular cancer to talk about fertility with their doctors early. This ensures they can protect their reproductive future before treatment.
Thanks to new reproductive technologies, even small sperm amounts can lead to pregnancy. With the right planning, many testicular cancer survivors can achieve their dream of fatherhood after treatment.
Follow-up Care and Monitoring
After treatment for testicular cancer, follow-up care is key. It helps catch any signs of cancer coming back early. It also looks at how treatment affects long-term health. Survivors must stay alert and keep up with doctor visits.
Regular Screening Schedule
The timing of follow-up visits varies based on the cancer’s stage and treatment. At first, survivors see doctors more often. Over time, these visits become less frequent.
| Time After Treatment | Recommended Check-up Frequency |
|---|---|
| 1-2 years | Every 2-3 months |
| 3-5 years | Every 4-6 months |
| 5+ years | Annually |
Long-term Health Considerations
Survivors of testicular cancer face special health challenges. These can include:
- Higher risk of heart disease
- Chance of getting other cancers
- Issues with fertility
- Hormonal problems
Staying healthy and making lifestyle changes are important. Survivors should talk to their doctors to create a follow-up plan that fits their needs.
Prevention and Self-Examination Techniques
Testicular cancer prevention begins with awareness and regular self-checks. Early detection is key to better outcomes. Learning how to do self-exams is important for catching problems early.
- Stand in front of a mirror and check for any swelling in your scrotum.
- Gently feel each testicle with both hands, rolling it between your fingers.
- Look for any lumps, changes in size, or unusual firmness.
- Check the epididymis, the tube behind each testicle, for swelling.
Do this monthly, best after a warm shower when your scrotum is relaxed. If you find any changes, see your doctor right away. Most lumps are not cancer, but it’s important to have them checked.
Living a healthy lifestyle also helps your testicular health. Eat well, stay active, and avoid tobacco. These habits improve your overall health, not just testicular health.
| Self-Examination Frequency | Key Areas to Check | When to Seek Medical Advice |
|---|---|---|
| Monthly | Testicles, Epididymis, Scrotum | Any lumps, swelling, or pain |
| After warm shower | Size, texture, firmness | Changes in testicular size or shape |
| Same time each month | Overall scrotal appearance | Persistent discomfort or heaviness |
Regular self-exams are a big step in preventing testicular cancer. This simple action can lead to early detection and better treatment results.
Impact on Quality of Life
Testicular cancer does more than harm your body. It changes your life in many ways. Let’s look at how it affects daily life.
Physical Effects
Testicular cancer can cause a lot of physical problems. Men might feel tired, in pain, or see changes in how they look. These issues can make it hard to work, enjoy hobbies, or connect with others. But, with the right care and support, many men get back to their normal lives.
Psychological Aspects
Testicular cancer brings up a lot of emotions. Men often feel scared, anxious, or depressed. They might also worry about how they look or their future health. Talking to a mental health expert or joining support groups can help. It’s okay to ask for help when you need it.
Social Support Systems
A strong support network is vital during cancer treatment. Family, friends, and other survivors can offer comfort and help. Online communities and special programs at hospitals also provide support. These resources are important for improving life during and after treatment.
FAQ
Q: What is testicular cancer?
A: Testicular cancer is a type of cancer that affects the testicles. It mostly happens in young men, between 15 and 35 years old. There are two main types: seminomas and nonseminomas, both germ cell tumors.
Q: What are the early warning signs of testicular cancer?
A: Look out for a painless lump or swelling in the testicles. You might also feel a heavy feeling in the scrotum or a dull ache in the lower abdomen or groin. If you notice any unusual changes, see a doctor right away.
Q: Who is at risk for developing testicular cancer?
A: Some risk factors include a family history of testicular cancer and undescended testicle(s). Certain genetic conditions and being Caucasian also increase the risk. But, many cases have no known risk factors, so regular self-checks are key.
Q: How is testicular cancer diagnosed?
A: Doctors use a physical exam, ultrasound, and blood tests to diagnose. They might also do a biopsy. Sometimes, a CT scan is needed to check if the cancer has spread.
Q: What are the treatment options for testicular cancer?
A: Treatment often starts with removing the affected testicle. Depending on the cancer type and stage, you might also have radiation, chemotherapy, or more surgery. Specialists in urologic oncology help decide the best treatment.
Q: Can testicular cancer affect fertility?
A: Yes, the cancer and its treatments can affect fertility. But, many men can father children after treatment. It’s wise to talk about fertility with your healthcare team before starting treatment.
Q: What is the survival rate for testicular cancer?
A: Testicular cancer has a high cure rate, over 95% in five years. Even if it spreads, modern treatments improve outcomes. Early detection and treatment are critical for these high survival rates.
Q: How often should I perform a testicular self-exam?
A: Do a testicular self-exam once a month. The best time is after a warm shower or bath. Knowing what your testicles normally feel like helps you notice any changes.
Q: What should I expect during recovery from testicular cancer treatment?
A: Recovery time varies based on treatment. After surgery, most men can get back to normal in 2-3 weeks. Chemotherapy or radiation recovery takes longer and may involve managing side effects. Emotional support is important during recovery.
Q: Are there any long-term health considerations for testicular cancer survivors?
A: Survivors should have regular follow-ups and watch for late effects of treatment. This includes cardiovascular issues or secondary cancers. A healthy lifestyle and talking openly with your healthcare team are key for long-term well-being.