Understanding and managing a vaginal yeast infection can be tough. It’s a common issue that many face, but few talk about. This article aims to help by explaining candidiasis clearly. We want to make talking about intimate health easier and less scary.

This guide is based on medical facts and written with your concerns in mind. It explores vaginal health in detail, separating real information from myths. We aim to break the silence around candidiasis and offer support to those seeking relief and understanding.
Key Takeaways
- Empathetic insights into the pervasive nature of vaginal yeast infections.
- Trusted resource for the identification and management of candidiasis.
- Illustrative guidance for recognizing and addressing symptoms.
- Thorough exploration of causes and effective treatment plans.
- Preventative strategies and debunking of common misconceptions.
Understanding Vaginal Yeast Infections
Yeast infections are common but often misunderstood. This section aims to explain what they are and how often they happen in women.
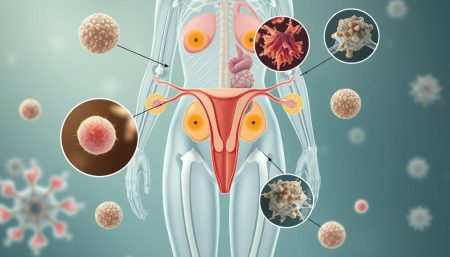
What is a Vaginal Yeast Infection?
A vaginal yeast infection is caused by too much Candida. Candida usually doesn’t harm us, but it can grow too much. This can cause itching, irritation, and unusual discharge. It’s important to know how Candida affects vaginal health.
The Role of Candida in Vaginal Health
Candida is a fungus found in our bodies, including the vagina. It’s usually harmless. But, if there’s an imbalance, it can grow too much and cause infections. Knowing about Candida helps keep the vagina healthy.
Statistics and Prevalence of Yeast Infections
Yeast infections are common among women. Many will get one at some point. Knowing this helps reduce the stigma around them. Here’s a table showing how common they are in different age groups:
| Age Group | Prevalence | Notes |
|---|---|---|
| 15-24 | 14% | Increased prevalence due to hormonal changes. |
| 25-34 | 20% | Highest prevalence, potentially linked to lifestyle and antibiotic use. |
| 35-44 | 18% | Decrease as hormonal levels begin to stabilize. |
| 45+ | 15% | Menopausal shifts potentially reducing Candida overgrowth. |
Common Symptoms of Vaginal Yeast Infections
Vaginal yeast infections, also known as thrush, can cause a lot of discomfort. They can affect your daily life. Knowing the symptoms early helps you get the right treatment quickly.
Identifying Symptoms of Vaginal Itching and Discomfort
Vaginal itching is a key sign of yeast infections. It can be very uncomfortable and may feel like burning. It often gets worse during urination or sex.
Spotting these signs early is important. It helps prevent the problem from getting worse.
Visual Signs of Vaginal Candidiasis
Thick, white discharge that looks like cottage cheese is a sign of candidiasis. The area around your vagina might also look red and swollen. It might even hurt when you touch it.
Watching for these changes is crucial. They show that you might have thrush.

When to Seek Medical Advice
If you notice symptoms like vaginal itching or unusual discharge, see a doctor. They can figure out what’s wrong and suggest the best treatment. Getting help early can stop the problem from getting worse and ease your discomfort.
The Causes Behind Yeast Overgrowth
Knowing the causes of vaginal yeast infection is key to stopping it. Yeast overgrowth comes from many things. This part talks about the main reasons for this common problem.
Hormonal shifts, like during the menstrual cycle, pregnancy, or menopause, change the vagina. This makes it easier for yeast to grow. Also, antibiotics mess with the balance of bacteria and yeast in the vagina.
- Hormonal changes that upset vaginal bacteria
- Antibiotics that lower lactobacillus bacteria
- A weak immune system that can’t control yeast
- Uncontrolled diabetes, as high sugar feeds yeast
Wearing tight clothes and using non-breathable fabrics also helps yeast grow. Knowing these points helps prevent infections and keep the vagina healthy.
Each factor changes the vaginal ecosystem’s balance. This is important to stop overgrowth and keep reproductive health good.
By tackling these causes, people can prevent causes of vaginal yeast infection. This protects their health.
Risk Factors for Developing Vulvovaginal Candidiasis
Knowing the risk factors for candidiasis is key to stopping and managing vulvovaginal candidiasis. Many things can make you more likely to get this condition. It affects women’s health all over the world.
Hormonal Changes and Yeast Infections
Hormonal shifts are a big deal when talking about vulvovaginal candidiasis. Things like pregnancy, menstruation, and hormonal birth control can change your vagina. This makes it easier for yeast to grow.
These changes mess with the good bacteria in your vagina. This can raise your chance of getting a yeast infection.
Impact of Antibiotics and Medications
Antibiotics and yeast infections are linked. Antibiotics kill bad bacteria but also harm good bacteria in your vagina. This can cause Candida to grow too much, leading to candidiasis.
It’s important to only take antibiotics when you really need them. Talk to your doctor about other options.
Some medicines, like steroids and immunosuppressants, can also weaken your immune system. This makes you more likely to get infections. Taking care of these medicines can help lower your risk.
Lifestyle Factors and Personal Hygiene
Your lifestyle affects your risk of vulvovaginal candidiasis. Bad diet, not enough sleep, and too much stress can weaken your immune system. This can lead to yeast overgrowth.
How you take care of yourself is also important. Too much or too little cleaning can upset the balance in your vagina. Use gentle, unscented products and wear cotton underwear to keep your vagina healthy.
To learn more about risk factors for candidiasis, check out reliable medical sources. They show how important it is to be aware and take steps to prevent this common condition.
Diagnosing Vaginal Yeast Infections
Getting a diagnosing yeast infections, also known as candidiasis, often begins with a doctor’s visit. It’s key to know how candidiasis diagnosis works. This includes several tests to make sure you get the right treatment.

When a doctor thinks you might have a yeast infection, they’ll ask about your symptoms and health history. They want to know about any past infections, medicines you’ve taken, and your overall health. This first step is important for what comes next.
| Diagnostic Tool | Description | Importance |
|---|---|---|
| Pelvic Examination | Visual and physical inspection of the vaginal area. | Identifies visible signs of yeast overgrowth and inflammation. |
| Microscopic Exam | Sample of vaginal discharge examined under a microscope. | Confirms the presence of Candida fungus. |
| Culture Test | Discharge is cultured to identify specific fungal species. | Helps tailor treatment by identifying the yeast strain. |
It’s very important to get a correct diagnosing yeast infections diagnosis. Wrong diagnoses can lead to treatments that don’t work. Each test is vital in the candidiasis diagnosis process. They help find the right treatment for you.
Knowing about these tests can make getting a diagnosis less scary. It helps you feel more in control of your health. By understanding these steps, you can be more involved in your care. This makes the whole process less intimidating and more empowering.
Professional vs. Home Treatments
Choosing between professional treatments and home treatments for yeast infections depends on the severity of symptoms and personal comfort. Each option has its benefits and drawbacks. These factors influence the decision for those suffering from this common condition.
When to Opt for Over-the-Counter Options
Over-the-counter yeast infection treatments are easy to find and work well for mild to moderate symptoms. They include antifungal creams, ointments, and suppositories. They are affordable and let patients manage their condition quickly without a doctor’s visit. But, it’s crucial to follow the directions to avoid resistance or misuse.
The Importance of a Doctor’s Diagnosis
While home treatments and over-the-counter yeast infection treatments are convenient, professional medical advice is vital. A doctor’s diagnosis confirms the symptoms are from a yeast infection, not something more serious. Professional treatments often start with accurate diagnostics, like lab tests to check for Candida and overall vaginal health.
Prescription Treatments and Their Effectiveness
Prescription treatments from healthcare professionals offer a stronger solution for severe or recurring yeast infections. These include potent antifungal medications, either topical or oral, proven to be effective. Professional treatments like this ensure thorough management of the condition, lowering the chance of it coming back.
| Treatment Type | Accessibility | Typical Use Case | Efficacy |
|---|---|---|---|
| Over-the-Counter | Highly accessible | Mild to moderate symptoms | Good for most cases |
| Prescription | Requires diagnosis | Severe or recurrent infections | Highly effective |
| Home Remedies | Readily available | Mild symptoms and maintenance | Varies widely |
Preventative Measures for Recurrent Yeast Infections
For many, recurrent vulvovaginal candidiasis disrupts daily life. It’s not just a medical issue, but a big problem. Preventing yeast infections is key. Here, we look at ways to lower the chance of these infections coming back.
- Eat a diet low in sugars and refined carbs to stop yeast from growing.
- Add natural yogurt and probiotics to your meals to keep vaginal bacteria in balance.
- Choose loose, breathable clothes and underwear made from natural fibers to keep moisture down.
- Use antibiotics wisely to avoid upsetting the body’s natural bacteria balance.
- Practice good hygiene but avoid over-washing or using harsh cleansers that can irritate the vagina.
Studies and trials back up these lifestyle changes. Here’s a table showing how these methods help manage recurrent vulvovaginal candidiasis.
| Preventative Measure | Effectiveness Percentage |
|---|---|
| Dietary Changes (Low Sugar Intake) | 75% |
| Probiotic Supplementation | 80% |
| Use of Breathable Fabrics | 65% |
| Limited Antibiotic Use | 70% |
| Appropriate Hygiene Practices | 68% |
These steps help those with recurrent yeast infections and give women control over their health. Always talk to a healthcare professional before making big health changes.
Myths and Misconceptions About Yeast Infections
We need to clear up yeast infection myths and misconceptions about candidiasis. These myths can confuse people. We want to fix these mistakes and break down vaginal health stigmas. This will help with treatment and emotional health.
Separating Fact from Fiction
Many think yeast infections mean you’re not clean. But, candidiasis is more about balance in your body. It’s important to know the truth to prevent and treat it right.
Common Misconceptions in Yeast Infection Treatment
Some think home remedies can fix yeast infections. While they might help a bit, seeing a doctor is key. They can give the right treatment to avoid bigger problems.
Addressing Stigmas and Women’s Health
Yeast infections make people feel ashamed. This stops them from getting help. We need to talk about this openly. This way, we can create a safe space for people to talk about their health without fear.
By fixing these myths, we give people the right info. This makes our community healthier. We can improve treatment and emotional health by educating and advocating together.
Conclusion
In this guide, we’ve looked at yeast infections in detail. We’ve covered their causes, symptoms, and how to manage them. Understanding the vaginal microbiome is key to beating this common problem.
Many things can upset the balance in the vagina, like hormones and antibiotics. Knowing this helps us prevent and treat yeast infections better.
The signs of a yeast infection are clear. Spotting them early helps manage them better. We’ve talked about treatments, both over-the-counter and prescription.
But, getting medical advice is crucial. It ensures you get the right treatment. Talking openly with doctors helps create a treatment plan that works for you.
We aim to clear up myths and help those dealing with yeast infections. Managing candidiasis is a shared journey. This guide is here to help you navigate it.
It’s important to remember the value of talking to medical professionals. They can offer advice that fits your specific needs.
FAQ
Q: What exactly is a vaginal yeast infection?
A: A vaginal yeast infection is caused by too much fungus in the vagina. This fungus is called Candida. It can make you feel itchy, burn, and have abnormal discharge.
Q: How does Candida normally function in vaginal health?
A: Candida is a yeast that’s usually in small amounts in the vagina. It’s kept in balance by good bacteria and the immune system. But, if this balance is broken, Candida can grow too much, causing a yeast infection.
Q: Are vaginal yeast infections common?
A: Yes, they are very common. The CDC says three out of four women will get a yeast infection at some point. Many women have it more than once.
Q: What are the primary symptoms of a vaginal yeast infection?
A: Symptoms include itching, irritation, and swelling in the vagina. You might also see a thick, white discharge that looks like cottage cheese. Pain when you pee or have sex is another symptom.
Q: What visual signs might indicate vaginal candidiasis?
A: Signs include a thick, white discharge without a strong smell. You might also see redness, swelling of the vulva, and a rash on the skin around the vagina.
Q: When should someone seek medical advice for a yeast infection?
A: If you have symptoms for the first time, they’re severe, treatments don’t work, or if you keep getting infections, see a doctor. Always get a healthcare provider’s advice for the right treatment.
Q: What causes yeast overgrowth and infection?
A: Yeast overgrowth can happen from taking antibiotics, hormonal changes, a weak immune system, diabetes, and high estrogen levels. This can be from pregnancy or hormone therapy.
Q: What are the risk factors for developing vulvovaginal candidiasis?
A: Risk factors include antibiotics, hormonal changes, and immune system problems. Lifestyle choices, like diet and hygiene, also play a role.
Q: How are yeast infections diagnosed?
A: Doctors usually diagnose yeast infections by looking, asking about your health, and your symptoms. Sometimes, they take a sample of vaginal discharge for lab tests to confirm Candida.
Q: Can over-the-counter treatments effectively manage yeast infections?
A: Yes, over-the-counter antifungal treatments work for many women with simple yeast infections. But, if you’re unsure or have a severe case, see a doctor first.
Q: Why is a doctor’s diagnosis important for treating yeast infections?
A: A doctor’s diagnosis is key to make sure you have a yeast infection and not something else. Different conditions need different treatments.
Q: Are prescription treatments for vaginal yeast infections effective?
A: Yes, prescription antifungal medications are very effective. There are different types, like pills, creams, and suppositories, chosen based on your condition.
Q: How can recurrent yeast infections be prevented?
A: To prevent them, keep good hygiene, wear cotton underwear, avoid douches and scented products, manage diabetes, and eat probiotic-rich foods or take supplements.
Q: What are the common myths surrounding yeast infections?
A: Myths include thinking yeast infections are from poor hygiene or that eating yogurt can cure them. These myths ignore the complex causes of yeast infections.
Q: How do misconceptions impact women’s health in the context of yeast infections?
A: Misconceptions can make women feel ashamed and avoid doctors. It’s important to talk openly about vaginal health to get the right treatment and reduce the emotional impact.