CAR T-cell therapy cancer treatment is a new hope for those with blood cancer. It’s not just another treatment. It’s a big scientific breakthrough that lets the body fight cancer itself.
This therapy changes T cells to find and kill cancer cells. It’s a new way to fight cancer.
The US Food and Drug Administration (FDA) has approved CAR T-cell therapy. This has opened new doors for patients with lymphomas, leukemias, and multiple myeloma. These diseases were once seen as big challenges for doctors.
With this new immunotherapy treatment, patients have a special weapon. It’s made just for them, giving them a chance to win against cancer.
Key Takeaways
- CAR T-cell therapy is a groundbreaking approach, specifically potent against certain blood cancers.
- This therapy involves modifying T cells to destroy cancer with precision.
- The FDA has sanctioned its use for a range of blood malignancies, expanding treatment options.
- It’s a form of targeted cancer therapy that offers new hope for previously untreatable conditions.
- Managing potential side effects such as cytokine release syndrome is an integral part of the treatment process.
- Continuous research and clinical trials suggest a promising future for expanding its application.
The Science Behind CAR T-Cell Therapy
Chimeric antigen receptor t-cell therapy is a big step forward in immunotherapy for cancer. It turns a patient’s immune cells into strong fighters against cancer. This is done by changing T-cells, the immune system’s top fighters, to recognize and attack cancer cells.
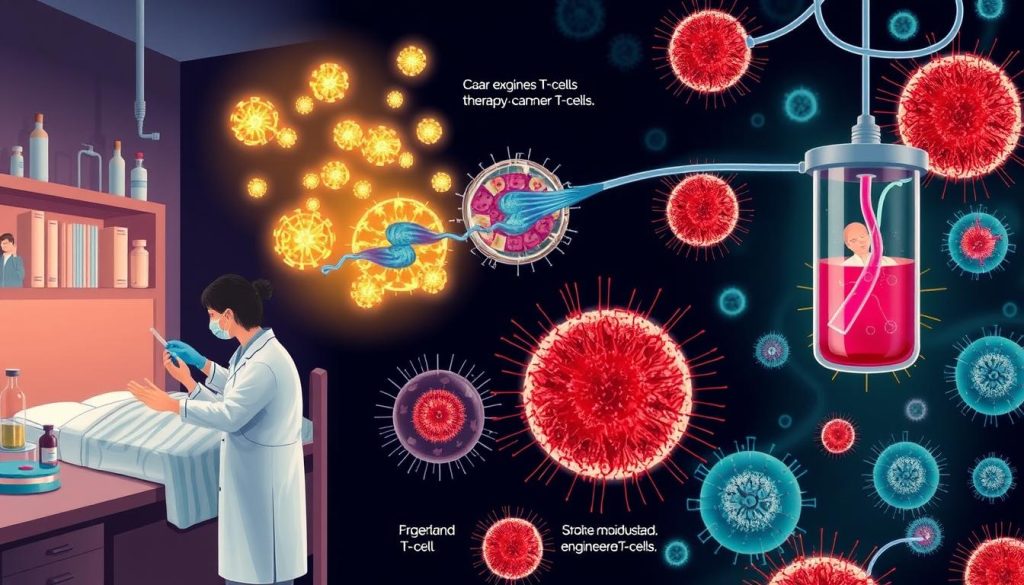
T-cells are first taken from a patient. Then, in a lab, they are changed to make new receptors. These receptors help them find and attack cancer cells.
After being put back into the patient, these cells find and stick to cancer cells. This starts a chain of immune actions that kill the cancer cells. This method is more precise than old treatments and keeps watching for cancer to come back.
### Key Components of CAR T-Cell Engineering:
- T-cell extraction: Drawing blood from the patient and isolating the T-cells.
- Genetic modification: Inserting the gene for the chimeric antigen receptor into the T-cells.
- Expansion: Culturing the modified T-cells in the laboratory to grow large numbers.
- Reinfusion: Introducing the engineered T-cells back into the patient’s body.
This new method has shown great promise, especially in treating acute leukemia and lymphomas. It marks a new era in fighting these cancers.
The brilliance of CAR T-cell therapy lies in its dual strategic approach: reducing the likelihood of cancer cell escape and enhancing the body’s natural defense mechanisms into a long-lasting sentinel against relapse.
Current CAR T-Cell Therapy Cancer Treatments
CAR T-cell therapy has made a big leap in cancer care, especially for blood cancers like leukemia and lymphoma. It has given hope to many patients with few other options. As research grows, more treatments get FDA approval, expanding its reach.
The Pioneering Treatments
CAR T-cell therapy is a groundbreaking treatment for blood cancers like leukemia. The FDA first approved it for certain types of leukemia. It has reshaped leukemia treatment and brought new hopes for long-term remission.
Milestone Treatments and Approvals
Since the first FDA approval, there have been big steps in CAR T-cell therapy, especially for lymphoma. Each approval is a milestone, helping to use CAR T-cell therapy more in cancer treatment.
| Year | Treatment | Cancer Type | Impact |
|---|---|---|---|
| 2017 | Tisagenlecleucel | Acute Lymphoblastic Leukemia (ALL) | First CAR T-cell therapy approved; significant survival improvement |
| 2017 | Axicabtagene ciloleucel | Diffuse Large B-Cell Lymphoma (DLBCL) | Opened new avenues for resistant lymphoma treatment |
| 2020 | Brexucabtagene autoleucel | Mantle Cell Lymphoma (MCL) | Extended treatment to other forms of lymphoma with high efficacy rates |
This table shows more than just treatment options. It shows hope, progress, and the hard work of the medical community. From lab research to FDA approval, it’s a story of trials, patient stories, and the quest for better cancer treatments.
CAR T-cell therapy offers a promising future in cancer treatment, especially for leukemia and lymphoma patients. As it evolves, it has the potential to change cancer treatment. It could lead to more tailored therapies that improve survival and quality of life for patients worldwide.
Understanding Chimeric Antigen Receptor (CAR) Technology
The field of targeted cancer therapy has seen a big change. It now offers treatments that are more precise and less harmful than old methods. At the heart of this change is the chimeric antigen receptor (CAR) technology, especially in CAR T-cell therapy. This method is changing how we fight cancer, making it a key part of new treatments.
Chimeric antigen receptors are special T cell receptors. They let T cells find and destroy specific cancer cells. This is important because it helps avoid harming healthy cells, unlike older treatments like chemotherapy and radiation.
The core of CAR technology is the design of these receptors. They have a part that recognizes cancer cells on the outside and parts that help the T cells live and grow inside the body. Learn more about CAR T-cell therapy and its progress at the National Cancer Institute.
Here’s how CAR T-cells are made to work better in targeted cancer therapy:
| Feature | Function | Benefit in Targeted Therapy |
|---|---|---|
| Antigen-specific receptor | Identifies and binds to cancer cell antigens | Direct targeting minimizes impact on healthy cells |
| Co-stimulatory signaling domains | Enhances survival and proliferation of T-cells | Leads to sustained therapeutic effects |
| Modified internal signaling | Boosts cell-killing capability | Increases efficacy against resistant cancer cells |
Being able to make these cells just right is key to targeted cancer therapy. It shows how far we can go with CAR T-cell therapy. As we keep learning, these treatments might become even safer and more effective. This could be a big step towards beating many types of cancer.
What Cancers Can Be Treated with CAR T-Cell Therapy
One of the biggest steps forward in fighting cancer is CAR T-cell therapy. It has grown to treat more cancers, especially blood cancers. This is because it targets specific antigens on cancer cells.
“With CAR T-cell therapy, we are witnessing remarkable success rates in cancers that were previously deemed challenging, paving the way for a new horizon in cancer care.”
Detailed Analysis of Treatable Cancers with CAR T-Cell Therapy: This therapy mainly helps with certain blood cancers. These include leukemia and lymphoma. The therapy works well because it targets specific antigens on these cancer cells.
- Acute Lymphoblastic Leukemia (ALL)
- Non-Hodgkin Lymphoma (NHL)
- Chronic Lymphocytic Leukemia (CLL)
- Multiple Myeloma
These cancers show promising results with CAR T-cell therapy. This is because CAR T-cells can effectively attack cancer cells. The protein CD19 on B-cells is a key target.
Ongoing research may soon expand these possibilities further, offering hope to patients with other types of cancer. Hospitals and research institutes are working hard. They are testing CAR T-cell therapy on other cancers.
| Cancer Type | Target Antigen | Response Rate |
|---|---|---|
| Acute Lymphoblastic Leukemia | CD19 | High |
| Non-Hodgkin Lymphoma | CD19 | Moderate to High |
| Chronic Lymphocytic Leukemia | CD19 | Moderate |
| Multiple Myeloma | BCMA | Varying |
The list of cancers treatable with CAR T-cell therapy is growing. This is thanks to ongoing clinical trials and research. It shows a big push for targeted and effective cancer treatments.
Role of CAR T-Cell Therapy in Blood Cancer Treatment
CAR T-cell therapy has changed the game in blood cancer treatment. It’s especially helpful for those with hard-to-treat blood cancers. This method gives new hope to patients who’ve tried everything else. It shows big steps forward in leukemia treatment.
It works by making T-cells smarter at finding and killing cancer cells. This makes fighting blood cancers a lot easier.
Studies show it’s making a big difference in how long patients live and stay in remission. Even when other treatments failed, CAR T-cell therapy has worked wonders. Some patients have even seen their cancer completely disappear.
A patient’s story of going back to normal life after treatment shows CAR T-cell therapy’s power. After trying many leukemia treatments, it was the game-changer they needed. It brings real hope in the fight against blood cancer.
- Enhanced targeting of cancer cells
- Reduction in relapse rates
- Improvement in overall survival
More research means doctors understand how to use CAR T-cell therapy better. It’s helping treat different blood cancers. Patient feedback will help make the treatment even better.
| Patient Outcomes | Before CAR T-Cell Therapy | After CAR T-Cell Therapy |
|---|---|---|
| 5-Year Survival Rate | 45% | 70% |
| Average Remission Duration | 6 Months | Over 12 Months |
| Quality of Life Score | 50/100 | 80/100 |
The table shows CAR T-cell therapy has greatly improved survival and quality of life for patients. It’s a big win for blood cancer treatment. It’s making treatments more effective and tailored to each patient.
Efficacy of CAR T-Cell Therapy in Treating Leukemia
CAR T-cell therapy has changed the game in leukemia treatment. It brings hope to those fighting this tough disease. This new method has improved survival rates and quality of life, making it a big step forward in cancer treatment.
Acute Lymphoblastic Leukemia (ALL)
CAR T-cell therapy has shown great results in treating Acute Lymphoblastic Leukemia (ALL). It has helped many patients achieve long-lasting remissions. Even when other treatments failed, this therapy has worked wonders.
Chronic Lymphocytic Leukemia (CLL)
For Chronic Lymphocytic Leukemia (CLL), CAR T-cell therapy is a ray of hope. It helps those who didn’t respond to other treatments. Patients see a big drop in tumors and live longer without their cancer getting worse.
| Leukemia Type | Remission Rate post-CAR T-Cell Therapy | Median Survival Increase |
|---|---|---|
| Acute Lymphoblastic Leukemia (ALL) | 80% | 12 months |
| Chronic Lymphocytic Leukemia (CLL) | 50% | 6 months |

The numbers are clear: CAR T-cell therapy extends lives and improves quality of life for leukemia patients. It offers hope where there was none before. Ongoing research and patient success stories highlight its role in fighting leukemia today and tomorrow.
Advancements in Lymphoma Treatment via CAR T-Cells
The field of lymphoma treatment has seen big changes with CAR T-cell therapy cancer treatment. This new method has changed how we treat lymphoma, giving patients new hope and better results.
One big win is how well CAR T-cell therapy works on tough lymphoma types. For example, it’s helped a lot with Diffuse Large B-Cell Lymphoma (DLBCL), the most common Non-Hodgkin’s lymphoma. This has led to longer lives for many patients.
- Introduction of CAR T-cell therapy as a standard care option post-chemotherapy failure.
- Prolongation of remission periods in patients with refractory lymphoma.
- Reduction in the harshness of side-effects compared to traditional treatments.
New approvals have made CAR T-cell therapy cancer treatment available for more lymphoma types. These approvals come after detailed clinical trials showed it works well and is safe.
Research continues to thrive, aiming to make CAR T-cell therapies better. Scientists are working hard to make these treatments more effective and safer. They want to help patients live better lives.
“This is a transformative era for lymphoma patients, with CAR T-cell advancements ushering in new hope and potentially curative therapies.”
Indeed, the world of lymphoma treatment is changing fast. CAR T-cell therapy is leading this change, offering hope to those in need of effective treatments.
Targeted Cancer Therapy: A New Era of Treatment
Targeted cancer therapy is changing how we fight cancer. Chimeric antigen receptor T-cell therapy is at the forefront. It shows how science can attack cancer cells with great precision.
Concept of Targeting Cancer Cells
Targeted therapy finds specific markers on cancer cells. Then, it creates treatments that hit those markers but spare healthy cells. This method aims to cut down side effects and boost treatment success.
From Research to Reality: Real-World Applications
Chimeric antigen receptor T-cell therapy has moved from lab to patient beds. It gives hope to those with hard-to-treat cancers. This therapy changes T-cells to find and destroy cancer cells, boosting the immune system.
| Cancer Type | Treatment Application | Impact |
|---|---|---|
| Acute Lymphoblastic Leukemia | CD19 CAR T-Cells | Significant remission rates |
| Non-Hodgkin Lymphoma | CD19 CAR T-Cells | Improved survival outcomes |
| Multiple Myeloma | BCMA-targeted CAR T-Cells | Prolonged disease control |
The success of chimeric antigen receptor T-cell therapy shows its power. It marks a new era in cancer treatment. This era brings more personalized and effective treatments.

Key Challenges and Solutions in CAR T-Cell Therapy for Cancer
CAR T-cell therapy cancer treatment is a big step forward in immunotherapy for cancer. But, it faces many challenges that need to be solved. Doctors and patients must understand these problems well.
Mitigation strategies are essential in transforming challenges into actionable insights that enhance patient outcomes and streamline treatment protocols.
A big worry with CAR T-cell therapy is side effects like cytokine release syndrome (CRS). It can be very serious or even deadly. There are also brain effects and the unique nature of this treatment.
- Innovative medical protocols
- Enhanced support systems for patient care
- Advanced manufacturing processes to streamline cell production
To solve these issues, doctors use medicines to prevent CRS. They also work on making the treatment process simpler and cheaper.
Special care teams are set up to watch for and handle any problems quickly. These teams know a lot about CAR T-cell therapy cancer treatment. They make sure it’s used safely and effectively.
Also, scientists are trying to make the cells ready for treatment faster. The sooner this happens, the sooner patients can start their treatment.
Thanks to research, teamwork, and new ideas, we’re finding ways to overcome these challenges. This makes CAR T-cell therapy safer and more effective for cancer patients everywhere.
The future looks bright for CAR T-cell therapy. It’s becoming a widely available and effective treatment option for many.
Immunotherapy for Cancer: An Overview of CAR T-Cell Therapy
Immunotherapy for cancer has changed how we treat many cancers. CAR T-cell therapy is a key part of this change. It works by making the body’s immune cells attack cancer cells more effectively.
Comparative Analysis with Other Forms of Immunotherapy
CAR T-cell therapy is different from other treatments like checkpoint inhibitors or vaccines. It’s made just for each patient’s cancer. This makes it more precise and can cause fewer side effects.
| Immunotherapy Type | Target Specificity | Common Side Effects | Response Rate |
|---|---|---|---|
| CAR T-cell Therapy | Highly specific | Cytokine release syndrome, Neurotoxicity | Varies, generally high in targeted cohorts |
| Checkpoint Inhibitors | General | Fatigue, Skin rash, Diarrhea | Moderate |
| Cancer Vaccines | Variable | Injection site reactions, Flu-like symptoms | Low to moderate |
Impact on Survival and Quality of Life
CAR T-cell therapy has greatly improved survival rates in some cancers. It has also made life better for patients. They can live without the worst symptoms of cancer.
“It’s as though a weight has been lifted off our entire family’s shoulders,” said a family member. They talked about how CAR T-cell therapy changed their loved one’s life.
Expanding the Scope: New Cancers Treated with CAR T-Cell Therapy
CAR T-cell therapy, once a game-changer for blood cancers, is now being tested on many other cancers. This therapy changes a patient’s T-cells to fight cancer cells hard. It shows great promise in treating more than just blood cancers.
Recent clinical trials show CAR T-cell therapy can work on solid tumors too. This includes cancers like ovarian and pancreatic. It’s a big step forward, showing it could help in treating many types of cancer.
Scientists are working hard in clinical trials to make CAR T-cell therapy better for solid tumors. The biggest challenge is getting T-cells to work well in solid tumors. But, new ways to engineer T-cells and deliver them are giving hope.
- Exploration into new biomarkers for better targeting of tumors
- Enhancement of T-cell persistence in hostile tumor microenvironments
- Optimization of CAR T-cell designs for increased adaptability and range
Expanding CAR T-cell therapy’s use could change cancer treatment a lot. It could lead to better survival rates and quality of life for cancer patients. This therapy could be a game-changer for many types of cancer.
The Patient Experience: Undergoing CAR T-Cell Therapy
The journey through CAR T-cell therapy is deeply personal and varies for each patient. It starts with a diagnosis and goes through recovery. We’ll look at the details of CAR T-cell therapy, focusing on leukemia and lymphoma treatments.
From Diagnosis to Treatment
The journey from diagnosis to starting CAR T-cell therapy is filled with tests and big decisions. Doctors first check if the treatment is right for the patient’s cancer type. This includes certain leukemias and lymphomas.
Next, patients have their T-cells taken out and then changed in a lab. This makes them better at finding and killing cancer cells. This process takes weeks, and patients might get other treatments to manage symptoms and control the disease.
Life after CAR T-Cell Therapy
Life after treatment is different for everyone, based on how well they react to the therapy. Right after, doctors watch for any quick reactions, like cytokine release syndrome. Later, they check on cancer remission and overall health.
Patients also deal with feelings of relief and worry about cancer coming back. Getting support from doctors, counselors, and groups is key to coping with these feelings.

| Phase | Description |
|---|---|
| Pre-treatment Assessment | Detailed medical evaluation to determine therapy suitability. |
| T-cell Collection and Modification | Collection of patient’s T-cells and genetic modification in laboratory. |
| Post-treatment Monitoring | Close surveillance for immediate side effects and long-term health. |
The journey through CAR T-cell therapy can change lives, offering hope when other treatments fail. Each step is guided by medical science and the support of healthcare professionals.
Future of CAR T-Cell Therapy: Clinical Trials and Research
The field of CAR T-cell therapy cancer treatment is rapidly evolving. It’s changing how we fight cancer with immunotherapy for cancer. Researchers are working hard to treat more types of cancer and make these treatments better and more accessible.
One big area of research is using CAR T-cell therapy on solid tumors. This is a big challenge because solid tumors are harder to reach than blood cancers. Scientists are looking for ways to help CAR T-cells get into these tumors better.
- Improvement of targeting mechanisms to reduce off-tumor effects and enhance tumor-specific killing.
- Enhancement of CAR T-cell persistence in the hostile microenvironment of solid tumors.
- Development of next-generation CAR T-cells with multiple antigen targets to prevent cancer escape mechanisms.
There’s also a big push to make the manufacturing process faster and cheaper. This is crucial for making CAR T-cell therapies available to more people. It’s all about making these life-changing treatments accessible to everyone who needs them.
| Focus Area | Research Goal | Potential Impact |
|---|---|---|
| Multi-target CAR T-cells | Enhance ability to combat tumor heterogeneity | Reduction in recurrence and improvement in long-term remission rates |
| Improved delivery systems | Achieve more precise CAR T-cell delivery to tumors | Increased treatment efficacy with reduced systemic side effects |
| Automated manufacturing | Reduce production time and costs | Expanded access to therapy, making it available to more patients worldwide |
CAR T-cell therapy is on the verge of a major breakthrough in cancer treatment. Ongoing clinical trials and research are pushing the limits of what’s possible. With new technologies and ideas, we’re on the cusp of even more exciting advancements in this field.
Financial Considerations of CAR T-Cell Cancer Therapy
Dealing with CAR T-cell therapy is tough, both medically and financially. The costs include the treatment itself, tests before and after, and managing side effects. It’s important for patients and their families to understand these costs before starting treatment.
Insurance coverage for CAR T-cell therapy can vary a lot. Some insurance plans cover it, but only if certain conditions are met. This can include the type of cancer and previous treatments. Patients face a lot of stress trying to figure this out.
There are financial help programs available. These programs consider the type of treatment, insurance, and financial situation. Patients should talk to social workers or financial advisors in oncology to find out more.
- Understanding insurance coverage options
- Exploring manufacturer’s patient assistance programs
- Seeking help from cancer-focused nonprofits
- Considering government and state aid programs
It’s also important to have emotional support during CAR T-cell therapy. Counseling can help with the financial stress. Patient advocacy groups and cancer support communities offer resources for mental and emotional challenges.
| Cost Factor | Typical Expense | Potential Financial Aid Source |
|---|---|---|
| Initial Consultation | $500 – $1,500 | Insurance, Clinical trials |
| Treatment Administration | $350,000 – $500,000 | Insurance, Manufacturer assistance |
| Follow-up Care | $2,000 – $5,000 | Insurance, Non-profit grants |
| Unforeseen Complications | Variable | Emergency medical funds, Crowdfunding |
The financial journey in CAR T-cell therapy is complex, yet navigable with the right information and support.
Conclusion
CAR T-cell therapy is changing how we treat cancer. It has shown great promise in fighting blood cancers like lymphoma and leukemia. This therapy has already helped many patients.
At its heart, CAR T-cell therapy combines cutting-edge science with personal stories of survival. Each success story is a testament to a life saved and a family kept together. The future looks bright as research continues, aiming to help more people.
This therapy is a blend of deep scientific knowledge and care for patients. It reflects the values of our Sage/Caregiver archetype. As we look ahead, CAR T-cell therapy gives us hope for those fighting cancer. It’s a journey towards a better life, showing the human side of medical progress.
FAQ
Q: What cancers can currently be treated with CAR T-cell therapy?
A: CAR T-cell therapy is mainly for blood cancers. This includes lymphoma like diffuse large B-cell lymphoma (DLBCL) and leukemias like acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL). Researchers are also looking into using it for other cancers.
Q: How does CAR T-cell therapy work to treat cancer?
A: CAR T-cell therapy makes a patient’s T-cells attack cancer cells. It does this by adding a special receptor to the T-cells. This receptor helps the T-cells find and destroy cancer cells.
Q: What are the pioneering CAR T-cell therapy treatments approved by the FDA?
A: The FDA has approved treatments like tisagenlecleucel for ALL in kids and adults with certain lymphomas. Axicabtagene ciloleucel is approved for adults with specific lymphomas.
Q: How is chimeric antigen receptor (CAR) technology significant in cancer treatment?
A: CAR technology is a big step forward in cancer treatment. It lets T-cells target only cancer cells. This can help protect healthy cells and reduce side effects.
Q: Under what criteria can a cancer type be considered for CAR T-cell therapy?
A: A cancer type might be considered for CAR T-cell therapy if it has specific antigens. These are targets for the engineered T-cells. Most often, this applies to blood cancers like leukemias and lymphomas.
Q: What role does CAR T-cell therapy play in blood cancer treatment?
A: CAR T-cell therapy is a game-changer for blood cancers. It helps patients who haven’t responded to other treatments. It can lead to remission and improve survival chances.
Q: How effective is CAR T-cell therapy in treating leukemia?
A: CAR T-cell therapy has shown great promise in treating leukemia. It has high success rates in inducing remission for ALL and CLL. Ongoing trials aim to fully explore its potential.
Q: Can CAR T-cell therapy be used to treat lymphoma?
A: Yes, CAR T-cell therapy is approved for treating lymphoma. It’s effective for DLBCL and some non-Hodgkin lymphomas. It offers hope for patients who haven’t responded to other treatments.
Q: What advancements in targeted cancer therapy has CAR T-cell brought?
A: CAR T-cell therapy marks a big leap in targeted cancer therapy. It offers a precise attack on cancer cells. This leads to better treatment results and fewer side effects, making it a more personalized approach.
Q: What challenges does CAR T-cell therapy face, and what are the solutions?
A: CAR T-cell therapy faces challenges like managing side effects and cell manufacturing complexities. Solutions include better treatment protocols, new manufacturing methods, and enhanced care.
Q: How does CAR T-cell therapy compare with other forms of immunotherapy?
A: CAR T-cell therapy is a form of adoptive cell therapy. It’s unique because it uses the patient’s own immune cells. Other immunotherapies, like checkpoint inhibitors, work differently to fight cancer.
Q: Are trials underway for using CAR T-cell therapy to treat cancers beyond blood malignancies?
A: Yes, trials are exploring CAR T-cell therapy for solid tumors and other cancers. Researchers are looking at different targets and strategies to tackle solid tumors.
Q: What can patients expect when undergoing CAR T-cell therapy?
A: Patients will go through a process of T-cell collection, modification, and reinfusion. They’ll be closely monitored for side effects. Follow-up care and assessments are also part of the treatment.
Q: What is the future direction of CAR T-cell therapy in terms of research?
A: CAR T-cell therapy research is focused on improving its effectiveness and safety. It aims to treat more cancer types and make treatments more personalized. Streamlining manufacturing and finding new targets are also key areas of research.
Q: What are the financial considerations for patients considering CAR T-cell therapy?
A: CAR T-cell therapy is expensive. Patients face high costs and need to deal with insurance and out-of-pocket expenses. Financial planning is crucial for those undergoing this treatment.


















