CAR T-cell therapy is a new way to fight cancer. It uses a patient’s immune system to find and kill cancer cells. This method is very precise. To start, doctors take a patient’s T-cells, which are important for fighting off infections. They then change these cells in a lab. The changed cells can now find and destroy specific cancer cells.
This treatment is special because it uses the patient’s own immune system. It has been very effective against some blood cancers. This includes acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL).
Researchers are now looking into using CAR T-cell therapy for other cancers too. This could give hope to people with aggressive or cancer that has come back. It might even lead to a better quality of life for these patients.
Introduction to CAR T-cell Therapy
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to target cancer cells. This method is different from traditional treatments like chemotherapy, which harm both cancer and healthy cells.
The idea of CAR T-cell therapy started in the 1980s. Back then, scientists were trying to make T-cells attack cancer. But it wasn’t until the 2010s that the first FDA-approved treatments were developed.
This therapy is special because it’s made just for each patient. It uses the patient’s own immune cells to create a strong treatment. This has worked well for some blood cancers, like acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCR).
Researchers are looking to use CAR T-cell therapy for more cancers. They want to make it safer and more effective. As it keeps improving, it gives hope for a more targeted cancer treatment.
“CAR T-cell therapy represents a new frontier in cancer treatment, giving patients a personalized way to fight cancer with their own immune system.” – Dr. Elizabeth Smith, oncologist
How CAR T-cell Therapy Works
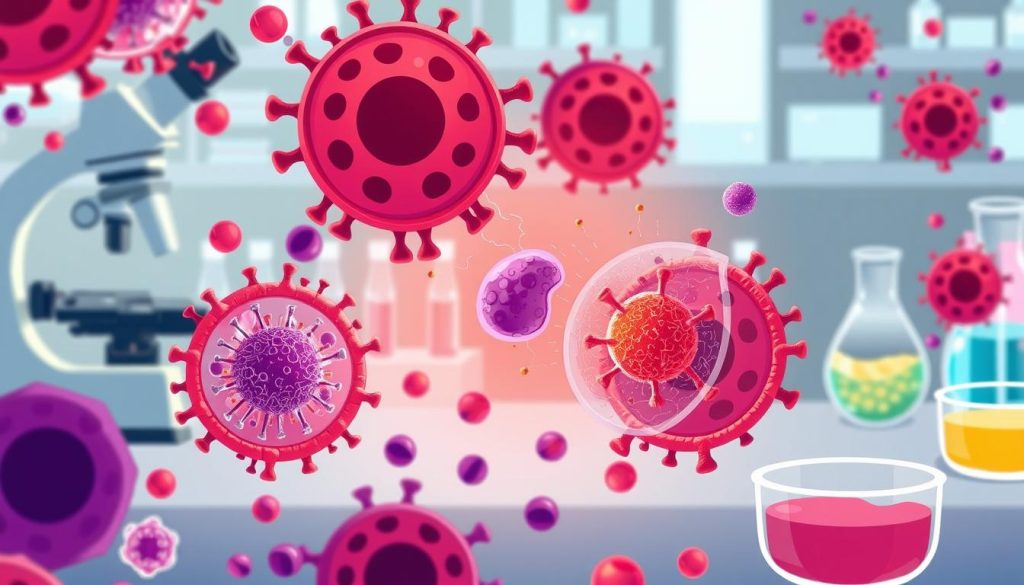
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. This method changes T-cells to find and destroy cancer cells.
Genetically Modifying T-cells
To start, a patient’s blood is taken to get T-cells. These cells are then changed in a lab. Scientists add a gene that lets the T-cells find cancer cells.

After, the T-cells are grown in the lab. This makes millions of CAR T-cells. These cells are ready to fight cancer when they are given back to the patient.
Targeting Cancer Cells with Chimeric Antigen Receptors
When the CAR T-cells are given back, they find and attack cancer cells. The CAR on the T-cells helps them find the cancer. This starts an immune response.
| CAR Component | Function |
|---|---|
| Antigen-binding domain | Recognizes and binds to specific cancer cell antigen |
| Transmembrane domain | Anchors the CAR to the T-cell membrane |
| Costimulatory domain | Enhances T-cell activation and proliferation |
| CD3ζ signaling domain | Triggers T-cell activation and cytotoxic activity |
The CAR T-cells release substances that kill cancer cells. They also multiply, creating more cells to fight cancer. This keeps going for a long time.
CAR T-cell therapy is a big step forward in cancer treatment. It uses the body’s immune system to target and destroy cancer cells.
The Process of CAR T-cell Treatment
CAR T-cell treatment is a detailed, multi-step process. It starts with collecting the patient’s T-cells. These cells are vital for fighting cancer.
T-cell Collection and Modification
The first step is collecting T-cells through leukapheresis. This involves drawing blood and separating T-cells from other components. The blood is then returned to the patient.
Next, the T-cells are genetically modified. They are made to recognize and attack cancer cells.
Lymphodepletion and CAR T-cell Infusion
Before infusing the modified T-cells, lymphodepletion is done. This reduces immune cells in the body. It helps the CAR T-cells work better.
Then, the CAR T-cells are infused into the patient. This process is like a blood transfusion and takes about an hour.
Monitoring and Follow-up Care
After infusion, patients are watched for side effects. Common issues include cytokine release syndrome and neurological problems. These can be treated with medical help.
Regular check-ups and tests are key. They help see how well the treatment is working and if cancer is coming back.
“The car t-cell treatment process is a revolutionary approach to cancer treatment that harnesses the power of a patient’s own immune system to fight cancer.”
A team of healthcare experts works together. They include oncologists, nurses, and support staff. Their goal is to give the best care to the patient.
Types of Cancer Treated with CAR T-cell Therapy
CAR T-cell therapy has shown great success in treating blood cancers. It uses the immune system to attack cancer cells. This gives hope to patients who have tried other treatments without success.
Currently, CAR T-cell therapy is mainly used for these blood cancers:
- Leukemia, such as acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL)
- Lymphoma, including diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma
- Multiple myeloma, a cancer of plasma cells in the bone marrow
There’s growing interest in using CAR T-cell therapy for other cancers. Researchers are looking into treating solid tumors like breast, lung, and prostate cancer.
“The success we’ve seen with CAR T-cell therapy in blood cancers like leukemia and lymphoma is truly remarkable. It gives us hope that we can eventually extend this treatment to a wider range of cancers and help more patients in need.” – Dr. Sarah Thompson, oncologist
As research continues, we might see CAR T-cell therapy used for more cancers. The future of cancer treatment looks bright, with personalized therapies like CAR T-cell therapy leading the charge.
Advantages of CAR T-cell Therapy
CAR T-cell therapy is a new way to fight cancer. It uses the body’s immune system to attack cancer cells. This could lead to long-term remission and a treatment plan made just for you.
Personalized Cancer Treatment
One big plus of CAR T-cell therapy is it’s made just for you. It changes your T-cells to find and kill cancer cells. This makes the treatment more effective and lowers the chance of it not working.
Harnessing the Power of the Immune System
This therapy uses your immune system to fight cancer. It makes T-cells that can find and destroy cancer cells. This way, it uses your body’s natural defense to fight cancer more effectively.
Potential for Long-term Remission
Some people have seen long-term remission from CAR T-cell therapy. In studies, many with certain blood cancers have stayed cancer-free for years after treatment.
| Advantage | Description |
|---|---|
| Personalized Approach | Tailored to the individual’s unique needs |
| Harnessing Immune System | Leverages the body’s natural defense mechanisms |
| Long-term Remission | Some patients experience complete remission lasting years |
CAR T-cell therapy is a hopeful new treatment. It’s personalized, uses your immune system, and could lead to long-term remission. It’s a big step forward in fighting cancer.
Risks and Side Effects of CAR T-cell Therapy
CAR T-cell therapy has shown great success in fighting some cancers. But, it comes with risks and side effects. Patients need careful monitoring and management to handle any problems that might come up.
Cytokine Release Syndrome (CRS)
Cytokine release syndrome is a serious reaction when the immune system gets too active. Symptoms can be mild, like flu, or very serious, like organ failure. These symptoms include:
- High fever
- Difficulty breathing
- Low blood pressure
- Rapid heartbeat
- Organ dysfunction
CRS usually starts within a week after treatment. It needs quick medical help. Treatment might include supportive care, steroids, and tocilizumab to block the syndrome’s effects.
Neurological Toxicities
Neurological side effects can happen with or without CRS. These can include:
- Confusion
- Delirium
- Tremors
- Seizures
- Speech difficulties
It’s important to watch the brain’s function closely during and after treatment. Managing these side effects might involve supportive care, steroids, and anti-epileptic drugs.
B-cell Aplasia and Immunodeficiency
CAR T-cell therapy targeting CD19 can sometimes remove healthy B-cells. This leads to a weak immune system and more infections. Patients might need long-term treatment with immunoglobulins to fight off infections.
| Side Effect | Symptoms | Management |
|---|---|---|
| Cytokine Release Syndrome (CRS) | Fever, difficulty breathing, low blood pressure, rapid heartbeat, organ dysfunction | Supportive care, steroids, tocilizumab |
| Neurological Toxicities | Confusion, delirium, tremors, seizures, speech difficulties | Supportive care, steroids, anti-epileptic medications |
| B-cell Aplasia and Immunodeficiency | Weakened immune system, increased susceptibility to infections | Long-term immunoglobulin replacement therapy |
The risks highlight the need for experienced healthcare professionals to administer CAR T-cell therapy in specialized centers.
Many see CAR T-cell therapy as a good option, despite the risks. It can offer long-term remission or even a cure for some cancers. Scientists are working to reduce the risks and side effects of this treatment.
Eligibility for CAR T-cell Therapy
When looking at CAR T-cell therapy eligibility, several factors are important. The type and stage of cancer, previous treatments, and the patient’s health are key. These aspects help decide if this treatment is right for someone.
The patient selection process is thorough. A team of healthcare experts evaluates each patient. They consider the patient’s medical history and current health to decide if CAR T-cell therapy is a good option.
Typically, patients with certain blood cancers, like leukemia and lymphoma, might be eligible. They must also have advanced cancer that hasn’t responded to usual treatments. Plus, they need to be in good health to handle the therapy’s side effects.
The criteria for CAR T-cell therapy can change based on the cancer type and the CAR T-cell product. For example, the table below shows the general criteria for two FDA-approved CAR T-cell therapies:
| CAR T-cell Therapy | Eligibility Criteria |
|---|---|
| Kymriah (tisagenlecleucel) |
|
| Yescarta (axicabtagene ciloleucel) |
|
“The decision to pursue CAR T-cell therapy should be made in close consultation with a healthcare team experienced in this innovative treatment approach.”
Each patient’s situation is unique when it comes to CAR T-cell therapy. A detailed evaluation by a specialized team is vital. This ensures the treatment’s benefits outweigh the risks for each patient.
Current Approved CAR T-cell Therapies
The FDA has approved several groundbreaking CAR T-cell therapies. These treatments use a patient’s immune system to fight cancer. Let’s explore the approved therapies.
Kymriah (tisagenlecleucel)
Kymriah, by Novartis, was the first CAR T-cell therapy approved. It treats:
- Patients up to 25 years old with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse
- Adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy
Yescarta (axicabtagene ciloleucel)
Yescarta, by Kite Pharma (a Gilead company), is another approved CAR T-cell therapy. It helps adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy. It treats:
- Diffuse large B-cell lymphoma (DLBCL) not specified
- Primary mediastinal large B-cell lymphoma
- High-grade B-cell lymphoma
- DLBCL arising from follicular lymphoma
Tecartus (brexucabtagene autoleucel)
Tecartus, also by Kite Pharma, is the latest FDA-approved CAR T-cell therapy. It treats adult patients with relapsed or refractory mantle cell lymphoma (MCL).
The table below summarizes the currently FDA-approved CAR T-cell therapies and their indications:
| Therapy | Indications |
|---|---|
| Kymriah | Pediatric and young adult B-cell ALL, adult large B-cell lymphoma |
| Yescarta | Adult large B-cell lymphoma |
| Tecartus | Adult mantle cell lymphoma |
These CAR T-cell therapies have shown great success in treating blood cancers. More therapies are expected to be developed and approved for different cancers.
Cost and Insurance Coverage for CAR T-cell Therapy
CAR T-cell therapy is a cutting-edge cancer treatment. But, it’s very expensive. The cost of car t-cell therapy can be between $373,000 and $475,000 per treatment. This makes it one of the priciest cancer treatments out there.
Several factors contribute to the high cost of CAR T-cell therapy:
- Personalized manufacturing process for each patient’s T-cells
- Complex genetic modification techniques
- Intensive medical care during and after treatment
- Research and development expenses
Even with the high cost, many insurance companies now cover CAR T-cell therapy for eligible patients. Insurance coverage can vary based on the plan and the patient’s health. Here are some key points about insurance coverage for CAR T-cell therapy:
| Insurance Type | Coverage Details |
|---|---|
| Medicare | Covers FDA-approved CAR T-cell therapies for certain cancers |
| Medicaid | Coverage varies by state, but many states cover FDA-approved treatments |
| Private Insurance | Coverage depends on the specific plan and medical necessity |
“We’re committed to ensuring that patients have access to this potentially life-saving therapy, and we’re working with payers to secure coverage and reimbursement.”
– Dr. David Chang, Kite Pharma
There are efforts to make CAR T-cell therapy more affordable and accessible. Companies, healthcare providers, and payers are working together. They aim to create new payment models and patient assistance programs. This will help more patients get this groundbreaking treatment.
Success Rates and Long-term Outcomes
As CAR T-cell therapy advances, patients and families want to know about success rates and long-term outcomes. This treatment is new but shows promise for some blood cancers. It can offer significant benefits.
One key benefit is its ability to induce long-lasting remissions. In trials, many patients have seen complete remissions lasting years. This gives hope for long-term survival.
The success of CAR T-cell therapy depends on the cancer type and patient’s health. For example, in some studies, it has a 40-50% success rate for relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
| Cancer Type | Complete Remission Rate | Median Overall Survival |
|---|---|---|
| DLBCL | 40-50% | 8-12 months |
| ALL | 70-90% | 12-18 months |
| Multiple Myeloma | 60-80% | 12-24 months |
Not all patients will respond to CAR T-cell therapy. Some may relapse after initial remission. The patient’s age, health, and cancer type can affect success.
“CAR T-cell therapy has the power to change cancer treatment. It offers hope to those with no other options. As we improve this technology, we’ll see better outcomes in the future.” – Dr. Sarah Johnson, oncologist
Research is ongoing to make CAR T-cell therapy more effective and safe. It aims to treat more cancers. As more data comes in, patients and their teams will make better decisions about this treatment.
Ongoing Research and Future Developments
The field of CAR T-cell therapy is growing fast. Scientists are working hard to make it safer and more effective. They aim to treat more types of cancer, not just blood cancers. They also want to make CAR T-cells more precise and reduce side effects.
One exciting area is making “off-the-shelf” CAR T-cell therapies. Right now, CAR T-cell treatments are very personal. They need a patient’s own T-cells. But scientists are trying to make universal CAR T-cells that can be made in large amounts. This could make treatments cheaper and more accessible.
“The future of CAR T-cell therapy lies in expanding its reach to more cancer types and developing off-the-shelf products that can benefit a larger number of patients.” – Dr. Sarah Johnson, Oncologist
Expanding CAR T-cell Therapy to Other Cancer Types
Researchers are now looking to use CAR T-cell therapy for solid tumors. They’re finding new ways to make CAR T-cells target specific cancer cells. Clinical trials are underway to test CAR T-cells in solid tumors like:
- Breast cancer
- Lung cancer
- Prostate cancer
- Ovarian cancer
- Pancreatic cancer
Improving Safety and Efficacy
To make CAR T-cell therapy better, scientists are trying different approaches. They’re working on:
- Creating more precise CAR T-cells to avoid harming healthy cells
- Adding safety features to control CAR T-cell activity
- Combining CAR T-cells with other treatments for better results
- Improving how CAR T-cells are made to make them stronger and last longer
Off-the-Shelf CAR T-cell Therapies
Creating off-the-shelf CAR T-cells is a big focus. These CAR T-cells come from healthy donors and are made to target cancer. The benefits include:
| Advantage | Description |
|---|---|
| Immediate Availability | Off-the-shelf CAR T-cells are ready for patients, cutting down wait times |
| Reduced Costs | Producing many off-the-shelf CAR T-cells can lower treatment costs |
| Standardized Manufacturing | Off-the-shelf CAR T-cells are made the same way, ensuring quality |
Comparing CAR T-cell Therapy to Other Cancer Treatments
When it comes to treating cancer, patients and their healthcare teams have several options to consider. Two common approaches are chemotherapy and stem cell transplants. A newer treatment called CAR T-cell therapy has also emerged as a promising alternative for certain types of blood cancers. Let’s explore how CAR T-cell therapy compares to these conventional treatments.
Chemotherapy targets rapidly dividing cells, including cancer cells and some healthy cells. This can cause side effects like hair loss, nausea, and fatigue. In contrast, CAR T-cell therapy is a more targeted approach. It genetically modifies a patient’s own immune cells to attack cancer cells. This precision may result in fewer side effects compared to chemotherapy.
Stem cell transplants, also known as bone marrow transplants, aim to replace damaged or diseased bone marrow with healthy stem cells. This procedure can be effective for certain blood cancers but carries risks such as infection and graft-versus-host disease. CAR T-cell therapy, on the other hand, uses the patient’s own T cells and does not require a donor. This may reduce some of these risks.
While both chemotherapy and stem cell transplants have been used successfully to treat various cancers, they may not work for everyone. CAR T-cell therapy has shown remarkable results in some patients with blood cancers who have not responded to other treatments. It is currently only approved for a limited number of cancer types.
The choice between CAR T-cell therapy, chemotherapy, and stem cell transplants depends on several factors, including the type and stage of cancer, the patient’s overall health, and personal preferences.
As research continues, scientists are working to expand the use of CAR T-cell therapy to other types of cancer. They aim to improve its safety and efficacy. In the future, this innovative treatment may become a more widely available option for patients battling various forms of cancer.
Patient Experiences and Testimonials
Real-life stories of car t-cell therapy show its power in fighting cancer. Sarah, a 42-year-old mom, talks about her journey: “After years of fighting leukemia, CAR T-cell therapy gave me a new chance. The treatment was tough, but my team and family helped me get through it.”
Mark, a 58-year-old who beat lymphoma, shares his story: “When my cancer came back, I lost hope. But then I learned about CAR T-cell therapy. It was hard, but seeing my T-cells fight cancer was amazing. Now, I’m in remission and loving every moment with my family.”
These stories highlight CAR T-cell therapy’s impact on patients’ lives. The treatment is tough, with side effects like cytokine release syndrome. Yet, the chance for long-term remission gives hope to those who’ve tried everything else. As research improves, more people will share their success stories, inspiring others.
FAQ
Q: What is CAR T-cell therapy?
A: CAR T-cell therapy is a new way to fight cancer. It uses the patient’s own immune cells, which are changed in a lab. This method helps the immune system attack cancer cells.
Q: How does CAR T-cell therapy work?
A: First, T-cells from the patient’s blood are collected. Then, they are changed in a lab to find and kill cancer cells. After that, these T-cells are given back to the patient to fight cancer.
Q: What types of cancer can be treated with CAR T-cell therapy?
A: CAR T-cell therapy is mainly for blood cancers like leukemia and lymphoma. But, scientists are also looking into treating other cancers with it.
Q: What are the advantages of CAR T-cell therapy compared to traditional cancer treatments?
A: CAR T-cell therapy is tailored for each patient. It uses the body’s immune system to fight cancer. This can lead to long-term remission without harming healthy cells.
Q: What are the most common side effects of CAR T-cell therapy?
A: Side effects include cytokine release syndrome, which can cause fever and breathing problems. Patients may also experience neurological issues and B-cell aplasia.
Q: Who is eligible for CAR T-cell therapy?
A: Who can get CAR T-cell therapy depends on their cancer type, previous treatments, and health. A team of doctors will decide if it’s right for each patient.
Q: What is the cost of CAR T-cell therapy, and is it covered by insurance?
A: CAR T-cell therapy is expensive, costing hundreds of thousands to millions of dollars. Insurance coverage varies. Efforts are being made to make it more affordable.
Q: What are the success rates and long-term outcomes of CAR T-cell therapy?
A: Success rates vary based on the cancer type and the patient. Some patients have had long-term remissions. More research is needed to understand its long-term effects.
Q: How does CAR T-cell therapy compare to stem cell transplants for treating blood cancers?
A: CAR T-cell therapy and stem cell transplants are both treatments for blood cancers. But, they work differently. CAR T-cell therapy uses modified immune cells, while stem cell transplants use donor stem cells. CAR T-cell therapy might be an option for those who can’t find a donor.
Q: Are there any patient stories or testimonials available about CAR T-cell therapy experiences?
A: Yes, many patients have shared their experiences with CAR T-cell therapy. Their stories offer hope and support to others considering the treatment. You can find these stories on websites and in materials from patient advocacy groups and cancer centers.